How to Reverse Prediabetes and Regain Your Health

When you learn you have prediabetes, it’s easy to feel overwhelmed. But the path to reversing it boils down to two fundamental things: adjusting what you eat and moving your body more. That’s really it. These changes help your body become more responsive to insulin, which is the whole game when it comes to getting your blood sugar back in check and heading off type 2 diabetes.
Making Sense of Your Prediabetes Diagnosis
Getting a prediabetes diagnosis isn't a life sentence—it's a wake-up call. Think of it as an early warning signal from your body, giving you a crucial window of opportunity to make some positive changes before things get more serious.
And you're definitely not alone. The number of people with prediabetes is growing worldwide. In fact, over 1.1 billion adults are now dealing with some form of impaired glucose regulation. You can read more about these global health trends00193-4/fulltext) to see just how common this has become.
At the heart of prediabetes is a concept called insulin resistance. Imagine insulin is the key that lets sugar (glucose) out of your bloodstream and into your cells for energy. With insulin resistance, your cells' locks get "sticky" and don't respond to the key as well. The sugar can't get in, so it builds up in your blood instead.
This infographic lays out exactly how that process works.
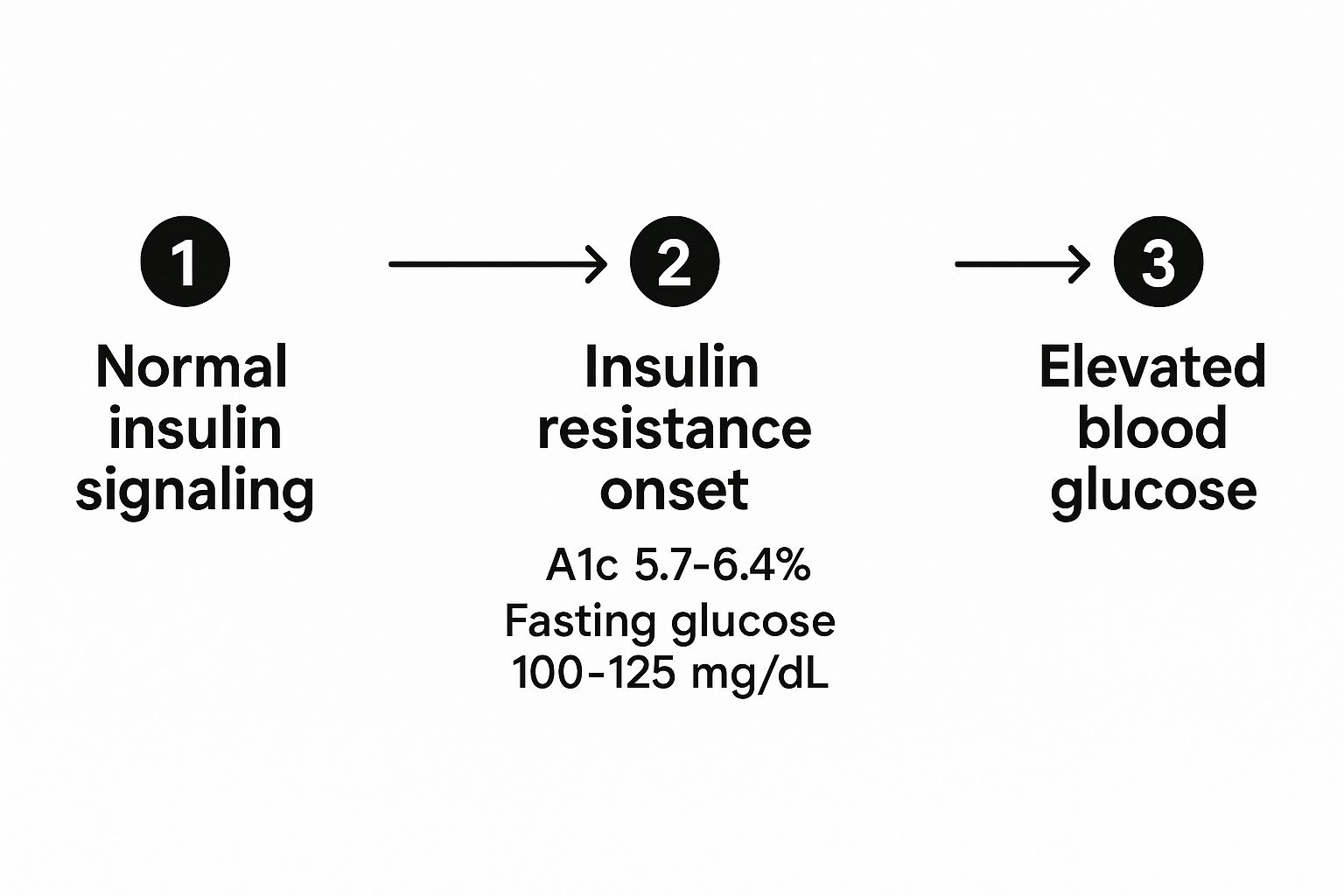
As you can see, the chart clearly shows the blood sugar thresholds that define prediabetes, so you can pinpoint exactly where you stand.
What Your Lab Results Actually Mean
When your doctor hands you that lab report, two numbers are front and center. Getting comfortable with what they mean is your first real step toward taking back control.
- A1c (Hemoglobin A1c): This is your average blood sugar over the last 2-3 months. Think of it as your long-term report card. An A1c under 5.7% is normal, while the prediabetes zone is 5.7% to 6.4%.
- Fasting Plasma Glucose (FPG): This is a snapshot of your blood sugar after an overnight fast (at least 8 hours). A normal result is under 100 mg/dL. The prediabetes range is 100 to 125 mg/dL.
These aren't just random numbers; they’re direct feedback from your body on how it's managing sugar. Seeing them creep into that prediabetes range is your cue to act.
This table breaks down the most important lifestyle changes into a simple, clear roadmap. It's your cheat sheet for what truly matters.
Your Core Actions for Reversing Prediabetes
| Strategy | Primary Goal | First Action Step |
|---|---|---|
| Dietary Changes | Stabilize blood sugar and reduce insulin spikes. | Swap one sugary drink (soda, sweet tea) for water or sparkling water today. |
| Increased Physical Activity | Improve insulin sensitivity so cells can use glucose more effectively. | Go for a 15-minute walk after your largest meal of the day. |
| Stress Management | Lower cortisol levels, which can raise blood sugar. | Practice 5 minutes of deep breathing or meditation before bed. |
| Prioritize Sleep | Improve hormonal regulation, including insulin and ghrelin (the hunger hormone). | Set a consistent bedtime and stick to it, aiming for 7-8 hours per night. |
These four areas are where you'll get the most bang for your buck. Don't try to tackle everything at once—just pick one "First Action Step" and build from there.
The most important thing to remember is that prediabetes is reversible. By focusing on sustainable changes to your diet, exercise, and daily habits, you absolutely can improve your insulin sensitivity and guide your blood sugar back to a healthy range.
This isn't about a crash diet or a temporary, all-out fitness blitz. It’s about building a healthier, more mindful relationship with food and movement that you can stick with for the long haul. The strategies in this guide are designed to be practical and empowering, giving you a clear path forward.
Building Your Prediabetes Reversal Diet
When it comes to reversing prediabetes, what you eat is your single most powerful tool. It's easy to get bogged down in complicated diet rules, but let's cut through the noise. We're going to focus on a simple, visual guide that makes healthy eating feel completely intuitive: the Plate Method.
This approach isn't about counting every last calorie. It’s about getting the right balance of nutrients to keep your blood sugar from spiking and crashing. Best of all, it’s a practical framework you can use for any meal, whether you’re cooking at home or eating out.
The Plate Method Explained
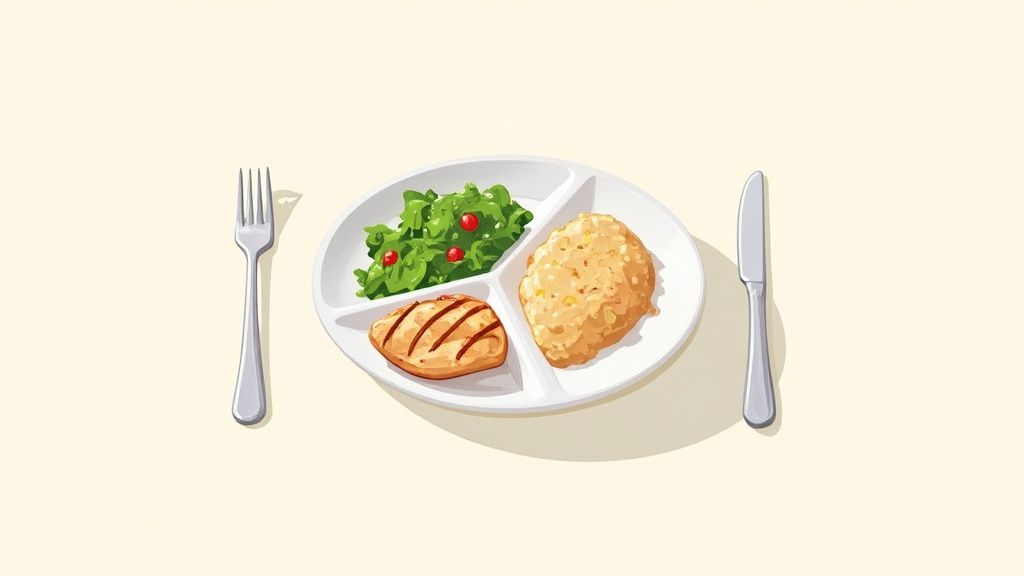
Think of your dinner plate as a pie chart. This simple mental picture is the key to building meals that get you closer to your health goals.
Here’s how to break it down:
- Half Your Plate (50%) Non-Starchy Vegetables: This is your base. Pile on colorful veggies like broccoli, leafy greens, bell peppers, or zucchini. They’re packed with fiber, vitamins, and minerals but are incredibly low in carbs and calories. They'll fill you up without messing with your blood sugar.
- One Quarter (25%) Lean Protein: Dedicate a quarter of your plate to a solid protein source. I’m talking about grilled chicken breast, baked fish, tofu, or a scoop of lentils. Protein is crucial for stabilizing blood sugar and keeping you feeling full, which helps fight off those cravings for sugary snacks later.
- One Quarter (25%) Complex Carbohydrates: The final quarter of your plate is for smart, fiber-rich carbs. Choose things like quinoa, brown rice, sweet potatoes, or whole-wheat pasta. Your body digests these slowly, giving you a steady stream of energy instead of a sharp glucose spike.
Using this method turns mealtime from a source of anxiety into a simple, repeatable habit for success.
By focusing on this balance—plenty of fiber from veggies, stabilizing protein, and slow-release carbs—you're creating a meal that works with your body, not against it. It's the most effective strategy for managing insulin response.
Putting It All Together: A Sample Day
So, what does this look like in the real world? Here’s a quick look at a typical day of eating to reverse prediabetes. You'll see how each meal sticks to that balanced plate idea.
A Simple Meal Plan
- Breakfast: Scrambled eggs (protein) with a handful of spinach mixed in, plus one slice of whole-grain toast (complex carb).
- Lunch: A big salad with grilled chicken (protein), loaded with mixed greens, cucumbers, and tomatoes (veggies), and a scoop of chickpeas (complex carb/fiber).
- Dinner: Baked salmon (protein) with a side of roasted broccoli and asparagus (veggies), and a small portion of quinoa (complex carb).
This structure does more than just help manage blood sugar; it ensures you’re getting a wide range of essential nutrients. The American Diabetes Association actually recommends eating patterns like the Mediterranean and plant-based diets, which naturally follow these same principles.
For more ideas, you can check out our guide on https://stopsugar.app/blog/what-foods-lower-blood-sugar. And if you’re plant-based, you might want to explore a low-carb vegetarian diet meal plan to find some great options that fit your lifestyle.
Making Movement Your Ally Against High Blood Sugar
While changing what you eat is a huge piece of the puzzle, movement is the other critical half of reversing prediabetes. Exercise is incredibly powerful because it helps your body use sugar for energy instead of letting it linger in your bloodstream. It actually makes your cells more receptive to insulin.
The key here isn't to suddenly start training for a marathon. Forget that "no pain, no gain" stuff. The real goal is to build a consistent fitness routine that you actually enjoy and can stick with for the long haul.
A smart approach combines two specific types of movement: aerobic exercise and strength training. This dynamic duo works together to supercharge your metabolism and improve how your body handles sugar.
The Power Couple: Cardio and Strength
Aerobic exercise, or cardio, is anything that gets your heart pumping—think brisk walking, cycling, or swimming. Strength training, on the other hand, is all about working your muscles against some kind of resistance, whether that's your own body weight, resistance bands, or a set of light dumbbells.
Here’s why you really want both in your corner:
- Aerobic Exercise: This is your immediate sugar-soaker. It uses up excess glucose in your bloodstream to fuel your activity. Even a simple walk after a meal can make a noticeable difference.
- Strength Training: This is your long-term strategy. Building even a little muscle gives your body more places to store glucose. Think of it as building bigger fuel tanks, so sugar has somewhere to go besides your blood.
The research on this is crystal clear. Getting at least 150 minutes of moderate-intensity activity per week (like that brisk walk) can slash your risk of developing type 2 diabetes by an astounding 58%. When you sprinkle in strength training a couple of days a week, those benefits get even better. You can read more about these CDC guidelines on diabetes prevention and see how they apply.
Here's an easy way to think about it: Cardio helps burn off the sugar that's in your system right now, while strength training builds the infrastructure to better manage sugar in the future. Together, they create a powerful defense against high blood sugar.
A Sample Weekly Fitness Plan to Get You Started
That 150-minute target might sound like a lot, but you don't have to do it all at once. Breaking it down into small, manageable chunks is the secret to success.
Here’s a simple schedule to show you just how doable this is:
| Day | Activity | Duration | Notes |
|---|---|---|---|
| Monday | Brisk Walk | 30 mins | A great way to unwind after dinner. |
| Tuesday | Strength Training | 20 mins | Focus on bodyweight moves: squats, push-ups, planks. |
| Wednesday | Rest Day | - | Take it easy. Maybe some light stretching. |
| Thursday | Brisk Walk or Bike Ride | 30 mins | Pick whichever one sounds more fun today. |
| Friday | Strength Training | 20 mins | Grab some light weights or resistance bands. |
| Saturday | Fun Activity | 60 mins | Go for a hike, take a dance class, or play a sport. |
| Sunday | Rest Day | - | Let your body recover and rebuild. |
This simple plan gets you to 160 minutes a week, hitting your goal with plenty of flexibility. If you're just starting, begin with 10-minute walks and gradually add more time and intensity as you feel stronger.
Remember, the best exercise plan is the one you actually do. Consistency is what will move the needle.
The Power of Monitoring Your Progress
You can't really improve what you don't measure. When you're working to reverse prediabetes, tracking your progress isn't about getting obsessed with numbers. It's about getting smart, powerful insights that keep you motivated and heading in the right direction. There’s nothing more encouraging than seeing tangible proof that your hard work is paying off.
This kind of feedback loop is what helps you truly understand your body's unique responses. For instance, you might discover that a brisk morning walk does more for your blood sugar than an evening stroll. These are the personal "aha!" moments that turn generic advice into a plan that actually works for you.
Key Metrics to Watch
To get a clear picture of how you're doing, it helps to focus on a few key areas. Each one tells a slightly different part of your health story.
- Occasional Blood Sugar Checks: Getting a simple glucometer and checking a few times a week can be incredibly revealing. Checking your levels before and after a new meal, for example, shows you exactly how that food affects you. We dive deeper into how a glucose monitor can support your health goals in our detailed guide.
- Weight and Waist Circumference: The number on the scale is just one piece of the puzzle. Don't forget to measure your waist. Losing inches there is a fantastic sign that you're shedding visceral fat—that's the dangerous kind that wraps around your organs and really drives insulin resistance.
Think of tracking not as a judgment, but as simple data collection. Every number, whether it’s what you hoped for or not, is just information. It’s a tool that empowers you to make an even better choice next time.
Consistently logging your new habits—what you eat, when you move—is what connects the dots. To help with this, you might want to use an effective habit tracker to record your daily efforts and start seeing those patterns emerge.
For example, an app like StopSugar is designed to bring it all together. You can log your meals, track your activity, and record your glucose readings in one place. When you see that skipping sugary sodas for a week not only stabilized your energy but also helped you drop a pound, it makes sticking with that new habit so much easier.
This is exactly how small, consistent actions create the kind of unstoppable momentum that can reverse prediabetes for good.
Mastering Lifestyle Habits for Long-Term Success

We've talked a lot about diet and exercise, and they are absolutely the stars of the show when it comes to reversing prediabetes. But two other factors are working behind the scenes that can quietly make or break your success: sleep and stress.
If you ignore them, you're essentially trying to fill a leaky bucket. You can put in all the hard work with food and fitness, but you won't get the results you deserve. That’s because these two elements have a direct line to your hormones, which are the master controls for your blood sugar and insulin sensitivity.
Why Your Sleep Schedule Matters
Think of sleep as your body's nightly maintenance crew. When you don't get enough quality rest, things start to go haywire. Just one or two bad nights can throw your system off, but chronic sleep deprivation is where the real damage happens.
In fact, a lack of quality sleep can slash your insulin sensitivity by over 30%. That’s a massive hit, and it forces your body to work so much harder to manage blood sugar. It's why aiming for a solid 7-9 hours of sleep isn't a luxury—it's a non-negotiable part of this plan.
Getting better sleep doesn't have to be complicated. Start with these simple, powerful habits:
- Stick to a Schedule: Try to go to bed and wake up around the same time every day. Yes, even on weekends. This single step works wonders for regulating your body's internal clock.
- Create a Restful Environment: Your bedroom should be a sanctuary for sleep—dark, quiet, and cool. A big one here: ditch the screens for at least an hour before bed. The blue light from your phone or TV can seriously mess with your body’s sleep signals.
- Wind Down: Don't just jump from a busy day straight into bed. Give your brain a chance to switch gears. Read a book (a real one!), take a warm bath, or listen to some calm music.
Taming the Stress Response
Chronic stress is the other silent saboteur. When you’re constantly on edge, your body pumps out a hormone called cortisol. Cortisol’s main job is to prep you for a "fight or flight" response, and it does this by dumping glucose into your bloodstream for a quick energy boost.
This is a brilliant survival mechanism if you’re actually running from a tiger. But when your stress is from traffic, deadlines, or daily worries, that extra sugar just hangs around, keeping your blood sugar levels high and constantly pressuring your pancreas.
Managing stress isn't just about feeling better in your head; it's a direct, physical intervention for your metabolic health. When you calm your nervous system, you reduce those cortisol spikes and give your body a fighting chance to regulate blood sugar the way it's supposed to.
You don't need a month-long yoga retreat to make a difference. Simple techniques can work wonders. For example, just five minutes of deep-breathing exercises can physically lower your cortisol levels and clear your mind.
The key is finding what works for you. Maybe it's a short walk outside, scribbling in a journal, or taking two minutes to think about things you're grateful for. Weaving these small moments of calm into your day creates a buffer against the pressures that can undo your hard work.
If you want to dive deeper into making these changes second nature, check out our guide on building healthy habits that last.
Here’s a rewritten version that sounds more human and natural, following all your requirements.
When to Chat with Your Doctor About Medication
Let's be clear: the changes you make to your diet and activity levels are, hands down, the most powerful tools you have for reversing prediabetes. But sometimes, even with your best efforts, your body might need a little extra help. That’s where medication can come in.
If your doctor brings it up, don't think of it as a setback. See it as adding another tool to your toolkit—a strategic way to get your blood sugar back on track and protect your health for the long haul.
The go-to medication for prediabetes is usually Metformin. It’s been around for a long time and works in a couple of key ways: it dials down the amount of sugar your liver releases and helps your body use the insulin it already makes more effectively. It’s not a magic pill that replaces a healthy lifestyle, but it can make all your hard work with food and exercise even more impactful.
Is Medication Right for You?
So, who is a good candidate for this? A doctor will look at your whole health picture, but certain factors might make Metformin a sensible option.
Your doctor might suggest it if:
- Your Body Mass Index (BMI) is 35 or higher.
- You are younger than 60.
- You're a woman who has had gestational diabetes in the past.
There’s some serious science to back this up. The famous Diabetes Prevention Program study—a major research effort—discovered that Metformin cut the risk of progressing to type 2 diabetes by a whopping 31% when paired with lifestyle changes. You can dive into the details of that study on the National Institute of Diabetes and Digestive and Kidney Diseases website.
Think of medication as a support crew for your new habits. It gives your metabolism a helpful nudge while you're busy building that solid foundation of healthy eating and regular movement.
Ultimately, the decision to add medication is a conversation, not a command. It’s something you and your doctor figure out together. Knowing what’s available means you can go into that chat feeling informed and ready to co-create a plan that truly works for you.
Of course. Here is the rewritten section with a more human, natural, and expert tone.
Got Questions About Reversing Prediabetes? We’ve Got Answers.
It’s completely normal to have a ton of questions when you first start trying to reverse prediabetes. Getting solid, practical answers can make all the difference, giving you the confidence to stick with the plan.
Let’s dig into some of the questions I hear most often.
How Quickly Will I Actually See Results?
This is probably the number one question, and the answer is probably sooner than you think. While getting your A1c back into the normal range is the long-term goal, you’ll likely feel better within just a few weeks.
Think clearer energy, less post-meal bloating, and a more even-keeled mood. Those are often the first clues that your new habits are working their magic.
As for the numbers, you can often see a real, measurable drop in your A1c levels after about three to six months of consistent effort. But remember, everyone is different. The key is to focus on the small, daily wins—the numbers will follow.
Do I Really Have to Give Up All the Foods I Love?
No, and you absolutely shouldn't. That all-or-nothing approach is a classic trap that almost always leads to burnout. This isn't about perfection; it's about finding a sustainable balance.
The goal is to make smarter choices most of the time, not to punish yourself. A great way to think about it is the 80/20 rule. If you're eating well 80% of the time, that leaves 20% for real life—a slice of birthday cake, your favorite pizza, a holiday meal—without the guilt.
Let's take pasta, for example. Instead of banning it forever, you could try a few simple swaps:
- Switch to a whole-wheat or chickpea version.
- Keep your portion size reasonable (think one cup, not a whole plate).
- Bulk up the meal with grilled chicken and a huge serving of roasted broccoli to balance out the carbs.
This kind of thinking is what makes a new lifestyle stick. It's about being consistent, not perfect.