What Causes Insulin Spikes? Your Guide to Balanced Sugar
Insulin spikes are your body’s reaction to a sudden flood of sugar in your bloodstream, a response mostly triggered by what you eat and how you live. Think of insulin as a traffic cop for your blood sugar, directing it out of the bloodstream and into your cells where it can be used for energy.
Your Body's Response to Sugar
When you eat—especially carbohydrates—your blood sugar levels naturally go up. In response, your pancreas releases insulin to get things back in balance.
This process is completely normal and necessary for life. The problem isn't the insulin itself, but the speed and size of its release.
Imagine you're filling a bathtub. A slow, steady trickle of water is easy to handle. But a sudden blast from a firehose is an emergency, forcing you to react quickly to prevent a flood.
That emergency reaction is the insulin spike. Your pancreas goes into overdrive, pumping out a huge amount of insulin to rapidly clear all that excess sugar from your blood. It's a powerful short-term fix.
But when these massive spikes happen over and over again, it’s like your body is constantly in emergency mode. Over time, your cells can start to ignore insulin's frantic signals, a condition known as insulin resistance. This guide will show you exactly what triggers these spikes and how you can encourage a more balanced, gentle response from your body.
Key Takeaway: The goal isn't to stop insulin release—that's impossible and unhealthy. The real aim is to avoid the dramatic, sharp spikes that put so much strain on your metabolic system.
For a personalized look at how your own body handles nutrients, a nutritional and metabolic assessment can offer some incredible insights that general advice just can't match.
Before we dive deep, let's get a high-level view of the main culprits behind these spikes. The table below gives a quick snapshot of the primary triggers we'll be exploring.
Key Triggers of Insulin Spikes at a Glance
| Trigger Category | Primary Examples | Impact on Insulin |
|---|---|---|
| Dietary Choices | Sugary drinks, refined carbs (white bread, pasta), processed snacks. | Causes the fastest and highest surge in blood sugar, demanding a large, rapid insulin release. |
| Meal Composition | Eating carbs alone, low-fiber or low-protein meals. | Without protein, fat, or fiber to slow digestion, sugar hits the bloodstream all at once. |
| Lifestyle Habits | Lack of physical activity, chronic stress, poor sleep. | These factors can impair your cells' sensitivity to insulin, requiring more of it to do the same job. |
Understanding what causes these spikes is the first real step toward gaining control, boosting your energy, and protecting your long-term health. Now, let's break each of these triggers down.
How High-Glycemic Carbs Fuel Spikes
Let's get one thing straight: not all carbs are the bad guy. But how they affect your blood sugar can be worlds apart. The biggest culprits behind those sharp, sudden insulin spikes are what we call high-glycemic carbohydrates. Getting a handle on these is your first real step toward managing your body's response.
Think of the Glycemic Index (GI) like a speedometer for your food. It measures how fast a carbohydrate-containing food dumps sugar into your bloodstream. High-GI foods are the Ferraris of the food world—they break down into glucose almost instantly, flooding your system and forcing your pancreas to pump out a huge wave of insulin to deal with the rush. That’s your classic insulin spike.
The Speed of Sugar Release
So, what makes a high-GI food different from a low-GI one? It all boils down to their structure. High-GI foods are usually heavily processed, which means they’ve been stripped of their natural fiber. Fiber is the body's built-in braking system for digestion.
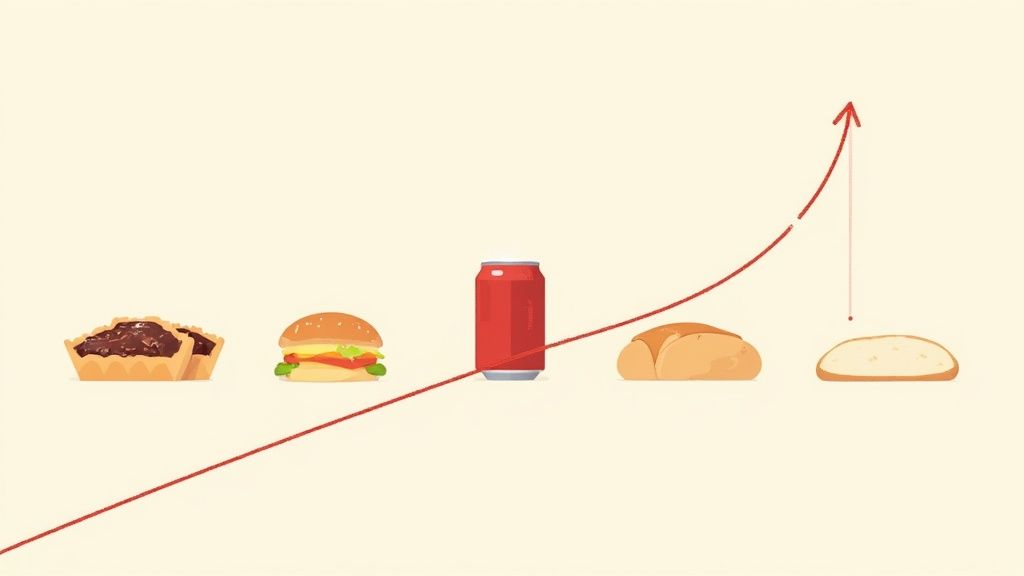
- High-GI Foods: We're talking about white bread, sugary breakfast cereals, pastries, and sweetened drinks. They barely need any work to digest, so they hit your bloodstream like a freight train.
- Low-GI Foods: Think whole grains, beans, lentils, and most vegetables. They're packed with fiber, which means they digest slowly and release sugar at a gentle, steady pace.
This visual breaks down how different food choices directly impact your body’s need for insulin.
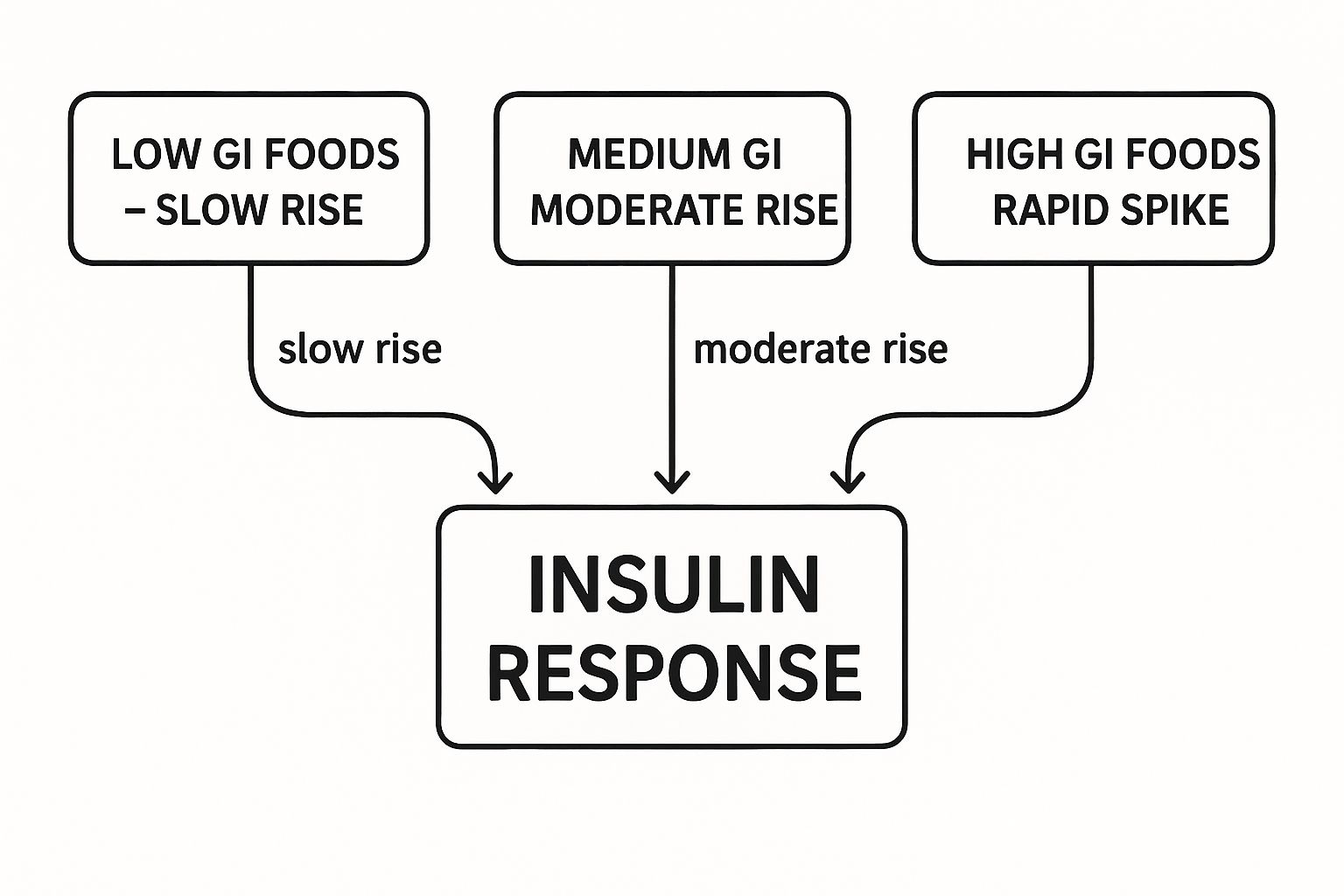
As you can see, a diet built around high-GI foods is a recipe for the kind of rapid spikes that really put a strain on your system over the long haul.
Why Refined Carbs Are the Main Culprit
Refined carbohydrates are without a doubt the primary offenders. When a grain is "refined," its two most nutritious parts—the bran and the germ—are stripped away. This is where almost all the fiber and nutrients live. Without that fiber, the carbohydrate becomes almost "pre-digested," ready for instant absorption.
For example, a bowl of cornflakes or a can of soda can send your blood glucose soaring by 30-50 mg/dL in as little as 15 to 30 minutes. Your body has no choice but to release a massive surge of insulin to bring things back under control. If you want to get into the nitty-gritty, you can learn more about this in our guide that explains the Glycemic Index in more detail.
A diet built on these fast-acting carbs means you’re triggering these intense insulin surges multiple times a day. This pattern is a huge driver behind the global rise in metabolic health problems.
Choosing better carbs isn't about cutting them out completely. It's about swapping the race cars for the reliable family sedans. By picking whole, fiber-rich foods, you’re giving your body the fuel it needs without sending it on a metabolic rollercoaster. It’s a simple switch, but it can make a world of difference for your energy levels and your health down the road.
How Your Body Weight Affects Insulin
When we talk about what causes insulin spikes, it's not just about the food you eat. Your overall lifestyle, especially your body weight, plays a massive role in how well your body manages blood sugar. The real troublemaker is visceral fat—the deep, internal fat that wraps around your organs.
This isn't just inactive baggage. Visceral fat is metabolically active, churning out inflammatory signals that essentially jam the communication lines between insulin and your cells. It’s like trying to talk to someone across a loud, crowded room. To get your message heard, you have to yell.
That's exactly what your pancreas has to do. It "yells" by pumping out way more insulin than usual just to get your cells to respond. This leads to bigger, sharper insulin spikes, even from a relatively normal meal. It's a tough cycle: the extra weight makes you more insulin resistant, and the high insulin levels tell your body to store even more fat.
Visceral Fat's Role in Jamming Insulin Signals
The connection between a high body mass index (BMI) and poor insulin response is crystal clear. Obesity is one of the biggest drivers of the frequent, high insulin spikes that pave the way for insulin resistance and type 2 diabetes. In fact, research shows that a high BMI is responsible for over 52% of the risk of developing type 2 diabetes. You can read more about the research linking BMI and diabetes risk.
This is why getting to a healthy weight is so fundamental for your metabolic health. It dials down all that inflammatory "noise," letting your cells hear insulin's signals loud and clear again. Your pancreas gets a much-needed break because it doesn't have to work overtime anymore. If you're working on weight management and want to cut back on sugar, our guide on the best sugar alternatives for weight loss is a great place to start.
The Power of Movement: One of the best things you can do to fight back is simply to get moving. Physical activity is a powerful antidote to insulin resistance.
Putting Exercise to Work for You
Exercise is a game-changer for blood sugar control, working in two brilliant ways to reduce the need for those big insulin surges.
- It boosts your insulin sensitivity. When you exercise regularly, your muscle cells become much more receptive to insulin. This means your body can get the job done with a smaller, more efficient release of insulin after you eat.
- It lets muscles take up sugar without insulin. During and right after a workout, your muscles can pull glucose straight from your bloodstream, no insulin key required. It's like they have a special side door that opens up, bypassing the main entrance completely.
Even something as simple as a brisk 15-minute walk after a meal can dramatically flatten the blood sugar curve that follows. By pairing smart food choices with consistent movement, you’re tackling one of the root causes of insulin spikes and building a much more resilient metabolism for the long run.
Uncovering Hidden Triggers Like Stress and Sleep
While most of us focus on diet and exercise, two other huge players often fly under the radar: chronic stress and poor sleep. These factors can trigger insulin spikes without you even eating anything, making them a critical piece of your metabolic health puzzle.
Imagine your liver has an emergency stash of fuel. When you're stressed out, your body floods with a hormone called cortisol. Think of cortisol as an alarm bell telling your liver to dump that stored sugar (glucose) into your bloodstream. It's an ancient "fight-or-flight" response getting you ready for action.
The problem is, your pancreas can't tell the difference between sugar from a donut and sugar from a stressful work meeting. It just senses high blood sugar and pumps out insulin to deal with it. This means that anxiety about a deadline can cause the exact same insulin spike as a sweet treat. Understanding these less obvious triggers is crucial; it's also worth exploring the key factors that cause heart palpitations, as many of them overlap with metabolic stress.
How a Bad Night's Sleep Fuels the Spike
A rough night of sleep can mess with your blood sugar in a surprisingly similar way. Research shows that just one night of bad sleep can make your cells more resistant to insulin the next morning. It’s like your cells are tired and sluggish—they don't hear insulin knocking at the door.
This forces your pancreas to work overtime, pumping out even more insulin to get the glucose into your cells. The result? A much higher insulin spike from the same breakfast you eat every single day.
Key Takeaway: Your mental and emotional state directly impacts your metabolic health. Managing stress and prioritizing sleep aren't just lifestyle luxuries; they are fundamental for keeping your blood sugar stable and preventing needless insulin spikes.
This connection shows why you can't just focus on your plate. You could have the most perfect diet in the world, but if you're constantly stressed and sleep-deprived, you'll always be fighting an uphill battle. True, lasting blood sugar control means looking at the whole picture—including the lifestyle habits that shape your body's internal environment.
The Long-Term Impact of Constant Spikes
So, what’s the big deal if you get a few insulin spikes here and there? A single one isn't going to cause any trouble. But when those spikes become a daily, repetitive pattern, the long-term consequences can be serious.
Think of it like constantly revving a car engine into the red zone. If you do it once, it’s probably fine. But do it multiple times every single day, and that engine is going to wear out.

In your body, that "engine" is your pancreas. When it’s forced to pump out huge amounts of insulin day after day, the cells that produce it (your beta cells) start to get exhausted. Over time, your body’s cells can also become less responsive to insulin’s signals. This is a condition called insulin resistance, and it's a huge stepping stone on the path to type 2 diabetes.
This pattern of chronic spikes, driven by our modern diet and lifestyle, isn't just a small issue—it’s a global health crisis. Since 1990, the number of adults with diabetes has more than quadrupled, now affecting over 800 million people worldwide. This incredible increase shows just how damaging repeated insulin surges can be on a massive scale. You can dig deeper into these trends on the World Health Organization's website.
It’s More Than Just Blood Sugar
The damage from constant insulin spikes goes way beyond your pancreas. Insulin is also your body's main fat-storage hormone. When insulin levels are always high, it’s like a constant signal telling your body to store any extra energy as fat. This makes it incredibly difficult to lose weight and much easier to gain it, especially around your belly.
This kicks off a nasty feedback loop. High insulin tells your body to store fat. That extra fat—especially visceral fat around your organs—makes your cells even more resistant to insulin. Your body's solution? Pump out even more insulin to get the job done.
The Vicious Cycle: Constant Spikes → Insulin Resistance → Higher Insulin Levels → More Fat Storage → Worsened Insulin Resistance
On top of all that, this ongoing metabolic stress creates a state of low-grade inflammation throughout your body. Chronic inflammation is a known trigger for a whole host of other serious health problems.
The Ripple Effect on Your Health
The long-term fallout from unchecked insulin spikes can be widespread, touching nearly every system in your body. It’s about so much more than just blood sugar.
- Cardiovascular Issues: Chronic inflammation and high insulin can damage blood vessels, which significantly increases your risk for heart disease.
- Weight Management Problems: With insulin constantly in fat-storage mode, burning fat becomes next to impossible, sabotaging even the best weight loss efforts.
- Hormonal Imbalances: Insulin doesn't work in a vacuum; it interacts with other key hormones. Chronically high levels can throw that delicate balance completely out of whack.
- Accelerated Aging: High blood sugar can lead to the formation of compounds called advanced glycation end products (AGEs), which damage cells and can speed up the aging process.
Understanding what causes these spikes is the first step. But recognizing these long-term risks is what makes it so clear: taking proactive steps to manage your blood sugar is one of the most powerful investments you can ever make in your future health.
Actionable Steps to Prevent Insulin Spikes
Knowing what causes an insulin spike is one thing, but actually doing something about it is where the magic happens. The good news is you can start balancing your blood sugar today with a few powerful, practical changes to what you eat and how you live.
These aren't about complicated rules or deprivation. They're simple, smart habits that work together to keep your metabolism humming along smoothly.
The single most effective strategy is to build your meals around what I call the "PFF" principle: Protein, Fat, and Fiber. Think of these three as the built-in braking system for any carbohydrates on your plate.
When you eat carbs all by themselves, the sugar hits your bloodstream like a freight train. But pair those same carbs with PFF, and you dramatically slow down digestion and the release of that sugar.
For example, instead of grabbing an apple by itself for a snack, add a small handful of almonds (that's your protein and fat) or a scoop of peanut butter. This one simple trick turns a potential sugar rush into a source of steady, sustained energy. No more spike, and no more crash.
Adopt Smarter Lifestyle Habits
What you do between meals matters just as much as what you eat during them. Your daily routines have a massive impact on how your body responds to insulin, and a few small, consistent tweaks can make all the difference.
- Take a Post-Meal Walk: This doesn't have to be a grueling workout. A simple 15-minute walk right after you eat encourages your muscles to pull glucose directly out of your bloodstream for fuel, taking a huge load off your pancreas.
- Prioritize Consistent Sleep: Seriously. Aim for 7-8 hours of quality sleep a night. Skimping on sleep makes your cells more resistant to insulin, forcing your body to pump out even more just to get the job done.
- Find Your Stress Solution: Chronic stress pumps out cortisol, a hormone that tells your body to release stored sugar into your bloodstream. Finding a way to unwind—whether it's meditation, deep breathing, or just a hobby you get lost in—is non-negotiable for metabolic health.
By weaving these food and lifestyle habits together, you're doing more than just fighting off spikes. You're building a stronger, more resilient metabolic system. Each balanced meal and post-dinner walk is a deposit into your long-term health account.
Getting these habits down also puts you in the driver's seat when it comes to cravings. For more specific tips, check out our guide on 8 ways to reduce sugar cravings that work for a few extra tricks up your sleeve.
If you feel you need a more customized plan, exploring personal nutrition coaching strategies can offer a roadmap built just for you. By making these small adjustments, you’re teaching your body to handle glucose more efficiently and turning that old cycle of spikes and crashes into a new one of balance and well-being.
Got Questions About Insulin Spikes? Let's Clear Things Up.
As you start wrapping your head around what causes insulin spikes, you'll probably have a few practical questions pop up. It's totally normal. Let's tackle some of the most common ones so you can feel confident putting this knowledge into practice.
But What About Healthy Foods? Can Fruit Cause a Spike?
Absolutely, and this is a great question. Even healthy foods like fruit can raise your blood sugar because, well, they contain sugar (fructose). But here’s the key difference: whole fruit is also loaded with fiber and water.
Think of that fiber as a built-in braking system. It slows down how quickly your body absorbs the sugar, leading to a much gentler, more gradual rise in blood glucose compared to, say, chugging fruit juice or eating a candy bar.
Want to flatten that curve even more? Try pairing your fruit with some protein or healthy fat. An apple with a scoop of peanut butter is a classic for a reason. That simple trick turns a potential sugar rush into steady, long-lasting energy.
The point isn't to be afraid of fruit. It's about being smart with how you eat it. A little protein or fat alongside it is a game-changer for keeping your blood sugar stable.
How Fast Will I Actually See a Difference?
You can start improving your insulin sensitivity a lot faster than you might think. Seriously. Just one solid workout can make your cells more receptive to insulin for up to 48 hours.
And when you start making consistent changes to your diet, getting more active, and prioritizing sleep, you can see real, measurable improvements in how your body handles sugar in just a few weeks. Don't aim for perfection—just focus on consistency. That's what truly moves the needle.