What Is Prediabetes and Can It Be Reversed?
Prediabetes is a critical health warning. It means your blood sugar levels are higher than they should be, but not quite in the range of a type 2 diabetes diagnosis.
Think of it as a yellow traffic light for your body. It's not a red light—it's a crucial heads-up, giving you a chance to slow down, reassess, and change course before your health hits a serious roadblock. The best part? It's often a reversible stage, putting you squarely in the driver's seat.
What Prediabetes Really Means for Your Health

So, what’s happening inside your body? The key concept to grasp is insulin resistance. Insulin is a hormone that works like a key, unlocking your cells to let in glucose (sugar) from your blood for energy. When you have prediabetes, your cells don't respond to that key as well as they used to.
To get the job done, your pancreas starts working overtime, pumping out more and more insulin to try and force those stubborn cells to open up. For a while, this brute-force approach works. But eventually, your pancreas can't keep up with the demand. As insulin resistance gets worse, that extra glucose has nowhere to go, so it just hangs around in your bloodstream, leading to those elevated blood sugar levels.
A Reversible Wake-Up Call
Receiving a prediabetes diagnosis isn't a life sentence. In fact, it's a powerful opportunity. Unlike type 2 diabetes, which is a chronic condition, prediabetes can often be completely turned around with focused lifestyle changes. It's your body's way of telling you it's time to pay closer attention to what you eat, how you move, and your overall well-being.
This isn't a small problem—it's a massive global health issue. A 2023 analysis found that in 2021, about 9.1% of adults worldwide, or roughly 464 million people, had impaired glucose tolerance, a hallmark of prediabetes. That number is expected to jump to 10.0%, affecting 638 million adults, by 2045. You can dig deeper into these trends in the full study published by the National Center for Biotechnology Information.
Prediabetes is often called a "silent" condition for a reason. Millions of people have it and have no idea. Since it rarely comes with obvious symptoms, getting screened and understanding your personal risk factors are absolutely vital for catching it early.
Understanding the Numbers
To know for sure, doctors rely on specific blood tests to measure your sugar levels. These tests place your results on a spectrum, with prediabetes sitting squarely in the middle between normal and diabetic.
To give you a clearer picture, here’s a quick guide to what the numbers mean. This table breaks down how doctors classify blood sugar levels, so you can make sense of your own test results.
Blood Sugar Status At a Glance
| Health Status | Fasting Plasma Glucose (mg/dL) | A1C Level (%) | What It Means |
|---|---|---|---|
| Normal | Below 100 mg/dL | Below 5.7% | Your body is managing blood sugar effectively. |
| Prediabetes | 100 - 125 mg/dL | 5.7% - 6.4% | Your blood sugar is elevated, indicating insulin resistance and a higher risk for type 2 diabetes. |
| Type 2 Diabetes | 126 mg/dL or higher | 6.5% or higher | Your blood sugar is consistently high, requiring medical management to prevent complications. |
Knowing where you land on this chart is your first real step toward taking action. Catching elevated blood sugar in the prediabetes range gives you the precious time you need to make changes that can safeguard your health for years to come and stop the progression to type 2 diabetes.
Understanding Your Personal Risk Factors
So, we know what prediabetes is. The next logical question is, "Why me?" Why do some people develop this condition while others don't? The answer usually isn't a single thing but a mix of factors that create your unique risk profile.
Think of it like being dealt a hand of cards. Some cards are genetic—you can't change them. But many other cards are based on your lifestyle, and you have a lot of say in how you play them. Understanding your full hand doesn't have to be scary. In fact, it's the first step toward taking control and making smart, proactive choices for your health.
Modifiable Risk Factors: The Ones You Can Change
Here's the good news: some of the biggest risk factors are completely within your control. These are the "modifiable" ones, meaning your daily habits and decisions can directly influence them for the better.
Excess Weight Carrying extra weight, especially around your middle, is one of the biggest drivers of insulin resistance. That belly fat, known as visceral fat, isn't just sitting there; it actively releases substances that interfere with how your body uses insulin. The great thing is that you don't need to achieve some "ideal" weight to see a huge benefit. Losing just 5% to 7% of your body weight can seriously improve your body's sensitivity to insulin.
Physical Inactivity Living a sedentary life is another major piece of the puzzle. When you're active, your muscles soak up glucose from your blood for energy, making them highly sensitive to insulin. When you're not moving much, your cells don't need that fuel, and they start to ignore insulin's signal. Think of regular exercise as a tune-up for your body's blood sugar management system.
Dietary Habits What you eat matters—a lot. A diet heavy on sugary drinks, processed foods, and unhealthy fats puts your system on a blood sugar roller coaster. These foods cause sharp spikes, forcing your pancreas to pump out more and more insulin to keep up. Over time, this constant demand can simply wear the system out.
Non-Modifiable Risk Factors: The Ones You Can't Change
Now for the factors you can't alter. While you can't change them, knowing about them is crucial. They provide important context and can be a powerful motivator to double down on the lifestyle habits you can control.
Your family history doesn't write your destiny, but it does give you a very important heads-up. It's a signal to be more proactive about the lifestyle factors you can control.
Here are the key risk factors that are simply part of your personal makeup:
- Family History: If type 2 diabetes runs in your immediate family (parents or siblings), your genetic risk is higher. You've essentially inherited a predisposition to insulin resistance.
- Age: Your risk naturally climbs as you get older, especially after age 45. Cellular changes over time can make your body less responsive to insulin.
- Ethnicity: Some ethnic groups, including African Americans, Hispanic/Latino Americans, American Indians, Asian Americans, and Pacific Islanders, have a genetically higher risk.
- History of Gestational Diabetes: For women, having diabetes during pregnancy significantly increases the risk of developing prediabetes and type 2 diabetes down the road.
By looking at both the factors you can change and those you can't, you get a clear, personalized picture of your risk. This isn't about placing blame; it's about empowerment. It turns vague health worries into a concrete action plan for prevention.
Recognizing the Subtle Signs of Prediabetes
One of the trickiest things about prediabetes is that it doesn't announce its arrival. There are no flashing lights or blaring alarms—just a quiet change happening inside your body. This is precisely why it’s earned the nickname "the silent condition," and it's the reason so many people have it without a clue.
But as blood sugar levels continue to creep up, your body may start sending out subtle hints. These whispers are all too easy to brush off as everyday stress or just part of getting older, but paying attention to them is one of the first steps toward taking control of your health.
Why Do These Symptoms Even Happen?
At their core, the early signs of prediabetes stem from one simple problem: too much sugar in the bloodstream. When your cells start ignoring insulin, that glucose can’t get inside to be used for fuel. It’s essentially locked out, left to build up in your blood and trigger a chain reaction throughout your body.
This extra sugar starts acting like a sponge, pulling water from your body’s tissues. Your kidneys then kick into overdrive, trying to filter out all that excess sugar and fluid, which leads directly to some of the most common symptoms.
Think of it this way: Imagine spilling a pile of sugar on your kitchen counter. It gets sticky and draws moisture from the air. In your bloodstream, that's essentially what excess glucose does—it messes with your body's fluid balance and makes your organs work harder to clean up the spill.
Common Signs to Watch For
While it's true that many people with prediabetes feel perfectly normal, others may begin to notice a few tell-tale changes. If any of these sound familiar, especially if you have other risk factors, it's worth listening to what your body is telling you.
- Increased Thirst and Frequent Urination: This is the classic duo caused by high blood sugar. As your kidneys flush out the extra glucose through urine, they take a lot of water with them. This dehydration makes you feel constantly thirsty, which leads to drinking more, which leads to… you guessed it, more urination. It's a frustrating cycle.
- Unexplained Fatigue: Your cells need glucose for energy. But with insulin resistance, that fuel can't get delivered properly. Even with plenty of sugar available in your blood, your cells are left starving. This energy deficit can leave you feeling drained and sluggish, even if you’re getting a full night's rest.
- Blurred Vision: High blood sugar levels can pull fluid into the lenses of your eyes, causing them to swell. This changes their shape and messes with their ability to focus, resulting in temporary blurriness. The good news is this usually corrects itself once your blood sugar stabilizes, but it's a definite red flag.
It’s incredibly important to remember that these symptoms alone aren't a diagnosis. They can be caused by a whole host of other issues. The only way to know for sure what's going on is to get tested by a doctor. Trying to self-diagnose can be misleading and might delay the care you really need, so a conversation with a healthcare professional should always be your first step.
How Doctors Diagnose Prediabetes and What the Numbers Mean
Getting a lab test can feel a little nerve-wracking, but understanding the results is the first step to taking control of your health. A prediabetes diagnosis isn’t just a hunch; it’s based on hard numbers from a few simple blood tests. Once you know what these tests measure and what your results mean, the whole process becomes much clearer—and you’ll feel more confident talking things over with your doctor.
The global focus on prediabetes is growing fast. In fact, the market for prediabetes diagnostics and management was valued at USD 8.81 billion in 2022 and is expected to hit USD 15.10 billion by 2032. This isn't just an economic trend; it shows a worldwide commitment to catching this condition early. You can dig deeper into these numbers from Coherent Market Insights.
This push for early detection is fantastic news because it gives you a crucial head start. Let's walk through the tests your doctor might use to check your blood sugar.
The Three Key Blood Tests for Prediabetes
Doctors have a few trusted ways to see how your body is handling sugar. Each test gives a slightly different view, but together, they paint a complete picture of your metabolic health.
1. The Hemoglobin A1C Test (HbA1c)
Think of the A1C as your "three-month blood sugar report card." It measures what percentage of your red blood cells are coated with sugar. Because red blood cells live for about three months, this test gives your doctor a long-term average of your blood sugar levels, smoothing out any daily spikes or dips. Best of all, there’s no fasting required.
2. The Fasting Plasma Glucose Test (FPG)
This test is more like a "snapshot" of your blood sugar. It measures the amount of glucose in your blood at a single moment after you’ve fasted (no food or drinks other than water) for at least eight hours. The FPG shows your baseline blood sugar level when your body is at rest.
The chart below shows exactly how the numbers line up, with prediabetes acting as the warning zone between normal and a full diabetes diagnosis.
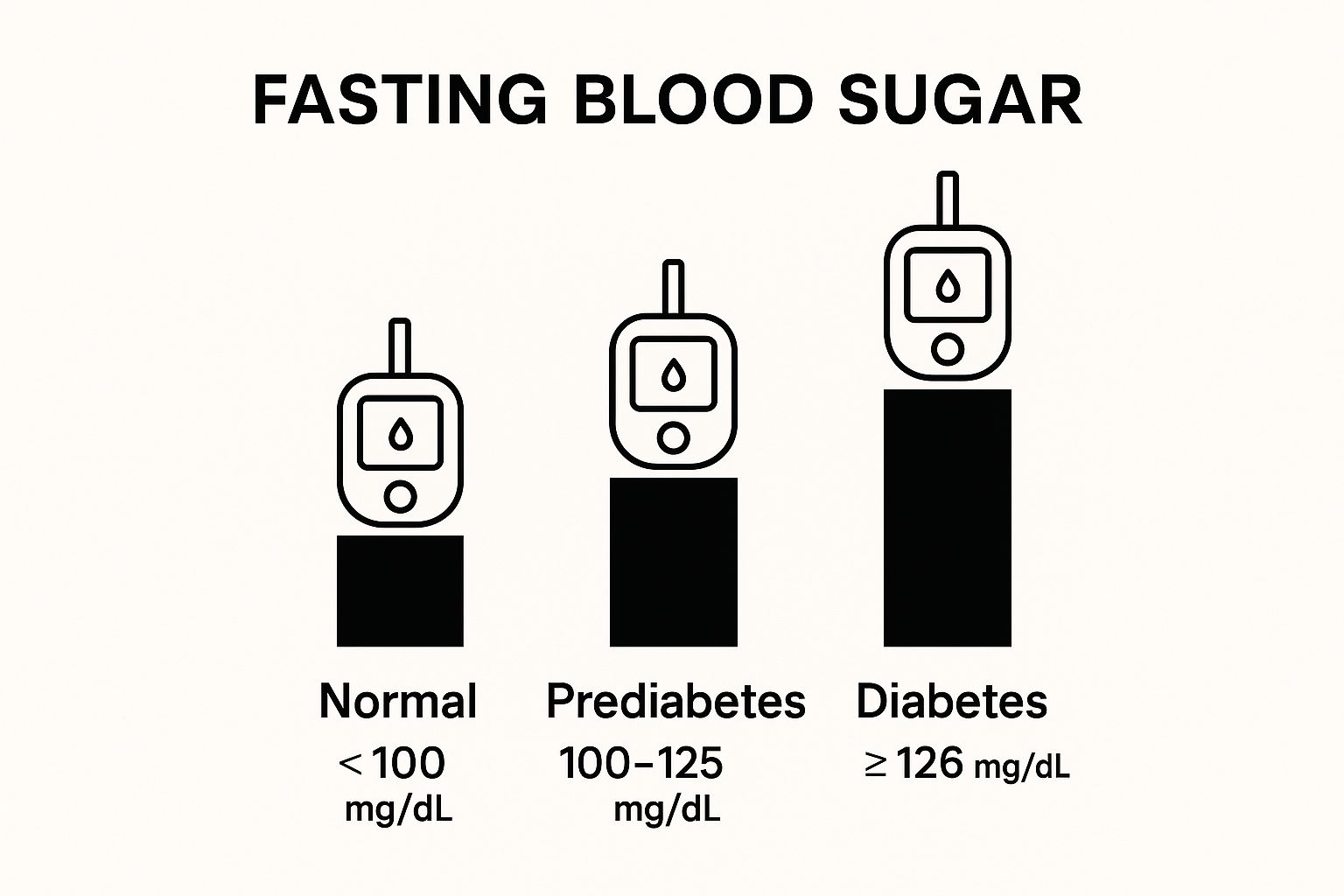
As you can see, that prediabetes range is a critical signal that it's time to make some changes before your blood sugar climbs higher.
3. The Oral Glucose Tolerance Test (OGTT)
You can think of the OGTT as a "stress test" for your metabolism. It’s designed to see how your body handles a sudden sugar load. First, a nurse will take a blood sample to get your fasting glucose level. Then, you'll drink a specially formulated sweet drink. Two hours later, they’ll test your blood again to see how efficiently your body cleared the sugar.
Understanding Your Prediabetes Test Results
Getting familiar with the different tests is the first part. The second, and most important, is knowing what your specific numbers mean. This is where you get the clarity needed to take action.
The table below breaks down the three main tests, what they measure, and the exact numbers doctors use to diagnose prediabetes.
| Test Name | What It Measures | Prediabetes Range | How to Prepare |
|---|---|---|---|
| Hemoglobin A1C | Your average blood sugar over the past 2-3 months. | 5.7% to 6.4% | None needed. |
| Fasting Plasma Glucose (FPG) | Your blood sugar after an 8-hour fast. | 100 to 125 mg/dL | Fast for at least 8 hours (water is okay). |
| Oral Glucose Tolerance (OGTT) | Your body's response to a sugary drink after a fast. | 140 to 199 mg/dL (at the 2-hour mark) | Fast for at least 8 hours and be prepared for a 2-hour test. |
If your results land in the prediabetes zone, don't panic.
A prediabetes diagnosis is a data point, not a destiny. Your test results are simply information—valuable information that gives you the opportunity to make positive changes and steer your health in a better direction.
Your doctor will likely want to retest to confirm the diagnosis. Once it's confirmed, you can start building a plan together. The best part is that now you have a clear reason and a measurable goal to work toward. To get going, check out our guide on 8 Proven Ways to Stabilize Blood Sugar Levels for some simple, effective tips.
Your Action Plan for Reversing Prediabetes
Getting a prediabetes diagnosis can feel jarring, but think of it as your body's most important early warning signal. It’s a clear opportunity to take charge and steer your health in a better direction, not a life sentence. And the best part? You have an incredible amount of power to turn things around. With a smart, practical plan, you can lower your blood sugar and slash your risk of developing type 2 diabetes.
This isn’t about making drastic, impossible changes overnight. Instead, the focus is on three solid pillars that support long-term health: smart nutrition, consistent physical activity, and effective weight management. Let’s break down how you can start building a healthier future, one small step at a time. Remember, the goal here isn’t perfection—it’s progress.
The Power of Modest Weight Loss
When it comes to reversing prediabetes, managing your weight is often the most powerful place to start. If you’re carrying extra weight, especially around your belly, losing even a small amount can make a world of difference in how your body uses insulin.
Research shows time and again that losing just 5% to 7% of your body weight can dramatically improve your insulin sensitivity. For someone who weighs 200 pounds, that’s only 10 to 14 pounds. This small, achievable change can be enough to nudge your blood sugar levels back into a normal range, essentially hitting the reset button on your metabolism.
This isn't about chasing some "ideal" weight from a chart. It's about finding a healthier, more comfortable weight for your body, which helps your cells start listening to insulin again.
Building a Nutrition Strategy That Lasts
Forget about those all-or-nothing diets that leave you feeling miserable. The real key to success is building sustainable eating habits you can actually stick with for life. Your goal should be to create balanced meals that nourish your body and keep your blood sugar stable, not leave you feeling deprived.
Here are a few core principles to get you started:
- Focus on Whole Foods: Prioritize foods that look as close as possible to how they came out of the ground or off the tree. This means loading up on fruits, vegetables, lean proteins like chicken and beans, and whole grains like oats and quinoa. They’re packed with fiber, which is your best friend for slowing down sugar absorption.
- Balance Your Plate: A great rule of thumb is to fill half your plate with non-starchy veggies (think broccoli, spinach, and bell peppers), a quarter with lean protein, and the final quarter with a high-fiber carbohydrate.
- Be Smart About Carbs: Not all carbs are the enemy! It’s about choosing the right ones. Opt for complex carbs like sweet potatoes and brown rice over refined carbs like white bread and pastries, as they release sugar into your bloodstream much more slowly.
- Practice Mindful Portions: Try using smaller plates and really tune into your body’s hunger and fullness cues. Eating slowly gives your brain time to register that you're satisfied, which is a simple trick to help prevent overeating.
Making smarter food choices also means tackling sugar cravings, which can be a huge hurdle. If you have a raging sweet tooth, there are great ways to get it under control. You can explore our expert tips on how to reduce sugar cravings naturally to help you stay on track.
Making Physical Activity a Daily Habit
You don’t have to become a gym rat or a marathon runner to see massive benefits. When it comes to exercise, the most important thing is consistency. The real secret is finding something you actually enjoy doing, because that’s what you’ll stick with.
Aim for at least 150 minutes of moderate-intensity activity each week. That’s just 30 minutes, five days a week.
What does "moderate intensity" feel like? You should be able to hold a conversation, but you shouldn't have enough breath to sing a song. Some easy ideas to get you started include:
- Brisk walking through your neighborhood or a local park
- Cycling on a stationary bike or outdoors
- Dancing to your favorite playlist in the living room
- Swimming or water aerobics
On top of that, try to add strength training at least two days a week. Building muscle is fantastic for blood sugar control because muscle tissue burns more glucose for energy, even when you’re just sitting on the couch.
The global impact of this condition is a stark reminder of why taking these actions is so critical. Prediabetes is the main runway to type 2 diabetes, a condition that affects millions. In 2021, an estimated 537 million adults were living with diabetes, and nearly half didn't even know they had it. As the International Diabetes Federation points out, it's a massive public health challenge. Your personal action plan is a powerful way to ensure you don’t become another statistic.
Answering Your Questions About Prediabetes
Hearing the word "prediabetes" for the first time can bring up a lot of questions and maybe a little worry. That's completely normal. Let’s walk through some of the most common questions people have, so you can feel more informed and in control of your health.
Can Prediabetes Actually Be Reversed?
Yes, it absolutely can. When we say "reversed," we mean bringing your blood sugar levels back down into the normal, healthy range. It’s not a one-time fix or a “cure” in the traditional sense, but rather a new, healthier status you achieve and maintain through consistent lifestyle habits.
Think of it as putting your risk for type 2 diabetes into remission. By making meaningful changes to what you eat, how much you move, and how you manage your weight, you can effectively hit the reset button on your blood sugar. The catch? You have to stick with these new habits to keep your levels from climbing back up.
Will My Doctor Put Me on Medication?
Probably not, at least not at first. Medication is rarely the first line of defense for prediabetes. The most powerful and proven treatment is lifestyle modification. Your doctor will almost always start by recommending changes to your diet and exercise habits, putting you in the driver’s seat of your own health.
In some cases, however, a doctor might suggest medication. This usually happens if you're considered very high-risk for developing type 2 diabetes, or if diet and exercise alone just aren't moving the needle enough. A common medication for this is metformin. Ultimately, this decision is made on a case-by-case basis, tailored to your specific health needs.
The goal is always to use the most effective and least intensive approach to get your blood sugar back in check. For the vast majority of people with prediabetes, that means lifestyle changes are the answer.
How Long Does It Take to Reverse Prediabetes?
There’s no magic timeline here—it’s different for everyone. How long it takes depends on your starting A1C and blood sugar levels, your personal risk factors, and—most importantly—how consistently you can stick with your new healthy routines. Some people see their numbers return to normal in just a few months. For others, it might take a year or more.
The real key is to focus on making sustainable changes you can live with long-term, not on a quick, temporary fix. Progress over perfection is the name of the game. Regular check-ins with your doctor will help you see how you're doing and keep you motivated. Even small, steady improvements add up to big results over time. A great place to start is learning how to stop sugar cravings naturally, which can make sticking to a healthier diet a lot easier.
Can Kids and Teens Get Prediabetes?
Unfortunately, yes. We're seeing more and more cases of prediabetes in children and adolescents. The same things that put adults at risk also affect younger people.
The biggest risk factors include:
- Being overweight or having obesity
- A family history of type 2 diabetes
- Not getting enough physical activity
If you have any concerns about your child's health, the best thing to do is talk to their pediatrician. The most effective approach is to build healthy habits as a family, creating a supportive home where everyone can stay healthy together.