Your Guide to Blood Sugar Mood Swings

Have you ever felt like you're riding an emotional roller coaster you didn't buy a ticket for? One minute you're fine, the next you're irritable, anxious, or just plain exhausted. These wild swings aren't just "in your head"—they're often a sign of blood sugar mood swings, a very real physical response to what's happening inside your body.
The Hidden Cause of Your Emotional Roller Coaster
Imagine your brain is like a high-end sports car. It needs a constant, steady supply of premium fuel to run smoothly. That fuel is glucose, which we get from our food.

When your glucose levels spike and then crash, it’s like flooding the engine one minute and running it on empty the next. The car is going to sputter, stall, and perform unpredictably. Your brain reacts in much the same way.
These fluctuations in blood sugar directly mess with your ability to regulate emotions, maintain focus, and keep your energy up. This isn't just a small annoyance; research confirms that both high and low blood sugar can trigger significant mood changes, including feelings of sadness and anxiety.
The Highs and Lows: It All Starts With Fuel
There's a straight line connecting what’s on your plate to how you feel. When you eat, your body breaks food down into glucose, which enters your bloodstream. In response, a hormone called insulin acts like a key, unlocking your cells to let the glucose in for energy. When this elegant system gets out of whack, your mood is one of the first things to go.
- High Blood Sugar (Hyperglycemia): After a meal packed with sugar or refined carbs, your bloodstream can get flooded with too much glucose. This overload often leaves you feeling agitated, anxious, and mentally foggy.
- Low Blood Sugar (Hypoglycemia): The "crash" after a big spike is when things get really rocky. When your glucose levels plummet, your brain panics because it's starved for fuel. It triggers a release of stress hormones like adrenaline, which can make you feel irritable, impatient, and even panicky.
Your emotions aren't random. They're often a direct signal about your body's internal state. Connecting the dots between your glucose levels and your mood is the first step to feeling more in control of both.
This constant cycle of spikes and crashes is why getting a handle on blood sugar mood swings is so important for your overall well-being. To really understand the whole picture, it helps to see what causes insulin spikes in the first place. Once you understand the root of the problem, you can start making changes to support stable energy and a more balanced mood.
How Glucose Levels Control Your Brain and Emotions
To get why blood sugar mood swings can feel so overwhelming, picture your brain as a supercomputer. It’s an incredibly powerful organ, but it's also a massive energy hog. Despite making up only 2% of your body's weight, your brain burns through about 20% of your daily energy. Its preferred fuel? Glucose.
Unlike your muscles or liver, your brain can't store much energy. It needs a steady, minute-by-minute supply of glucose delivered directly from your bloodstream to keep running smoothly. When that fuel delivery gets choppy—either from a sudden flood or a sudden shortage—the whole system starts to glitch. This directly affects everything from your concentration to your emotional state.
The Problem With Too Much Fuel
When you eat a meal heavy in refined carbs or sugar, your bloodstream can get saturated with glucose. This state, known as hyperglycemia, puts your brain under serious strain. Think of it like pouring way too much gasoline into an engine—it gums up the works. High glucose levels can spark inflammation and oxidative stress, which can damage brain cells and mess with their communication signals.
This isn't just some silent, microscopic process. You feel it.
- Brain Fog: Thinking can feel slow and sticky, as if you're trying to wade through mental mud.
- Anxiety and Agitation: The internal chaos often shows up on the outside as restlessness, a short fuse, or a persistent feeling of anxiety.
- Fatigue: It’s ironic, but a sugar rush is almost always followed by a crash. You feel drained as your body works overtime to deal with the glucose overload.
This constant high-alert state drains your mental batteries, leaving you feeling exhausted and emotionally raw. The first step to avoiding this is understanding which foods are the biggest culprits. A great way to start is by learning what is the glycemic index and how it rates foods based on their blood sugar impact.
When the Fuel Tank Runs Empty
The real emotional rollercoaster often begins during the "crash," also known as hypoglycemia. After a huge sugar spike, your body can overcompensate by releasing too much insulin, which causes your blood sugar to plummet. Suddenly, your brain is starved of its primary fuel, and it treats this situation like a five-alarm fire.
It immediately hits the panic button, flooding your system with stress hormones.
Your body’s reaction to low blood sugar is a deep-seated survival instinct. It triggers the 'fight-or-flight' response, preparing you to handle a threat—even if the "threat" is just a lack of fuel.
This hormonal cascade is what makes a sugar crash feel so intense and awful. Let's look at the two main hormones involved and what they do to your mood:
- Adrenaline: This is your first-responder hormone. It’s responsible for the classic crash symptoms: shakiness, a pounding heart, and sudden sweating. Emotionally, this surge feels like instant irritability, impatience, or even a wave of panic.
- Cortisol: Often called the "stress hormone," cortisol's job is to help your body tap into its energy reserves. But when cortisol levels stay high, they can disrupt your brain's feel-good chemicals, like serotonin and dopamine. This can leave you feeling sad, down, and emotionally flat.
This one-two punch of hormones is why a simple drop in blood sugar can feel like a full-blown emotional crisis. You’re not just "being cranky"—your body is reacting to what it perceives as a genuine emergency. This is the core reason why learning to stabilize your blood sugar is one of the most powerful things you can do for your emotional well-being.
Recognizing the Signs of Blood Sugar Swings
The first step in managing blood sugar mood swings is learning to recognize them when they happen. These shifts aren't just random feelings—they're direct signals from your body about its fuel levels. Once you start connecting the physical sensations with your emotional state, you'll begin to see clear patterns.
Think of yourself as a detective. When a wave of irritability suddenly hits, instead of just chalking it up to a bad day, ask yourself: What did I eat an hour ago? Am I also feeling a bit shaky or tired? This kind of self-awareness helps you get to the root cause of your emotional roller coaster.
The link between blood sugar and mood is nothing new. Scientists have been studying it since the 1930s, observing how both high and low glucose can trigger negative emotions like anxiety and agitation. In fact, severe fluctuations were once called 'brittle diabetes,' and even the act of checking blood sugar could bring on feelings of stress or failure. You can learn more about the history and modern understanding of glucose and mood from this study.
Spotting the Signs of Low Blood Sugar
Low blood sugar, or hypoglycemia, is that classic "crash" that often follows a sugar high. When your brain's fuel supply plummets, your body hits the panic button and releases stress hormones like adrenaline. This is what causes those intense, hard-to-ignore physical and emotional symptoms.
The feeling is often abrupt and overwhelming, making it difficult to think straight. You might experience:
- Sudden Irritability: Small annoyances suddenly feel like major crises. Your patience vanishes in an instant.
- Anxiety or Nervousness: A sense of unease or panic can wash over you for no apparent reason.
- Shakiness and Dizziness: You might notice your hands trembling, or you could feel lightheaded and unsteady on your feet.
- Intense Hunger or Cravings: This isn't just regular hunger; it’s a powerful, urgent need to eat, usually something sweet.
This infographic shows how physical and emotional symptoms stack up during blood sugar swings.
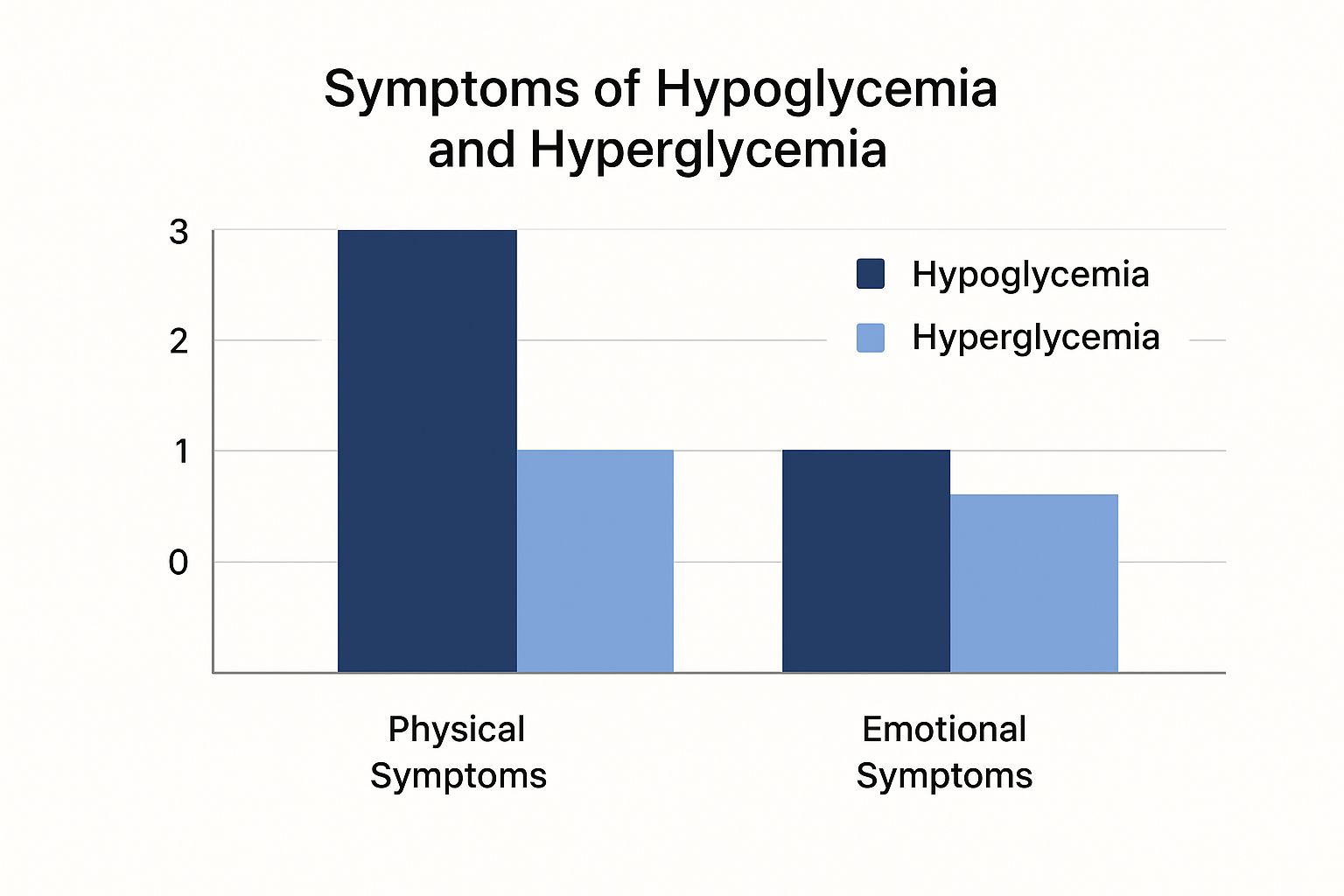
As you can see, while both high and low blood sugar cause emotional distress, the physical warning signs of a crash are often much more immediate and intense.
Identifying High Blood Sugar Symptoms
High blood sugar, or hyperglycemia, brings on a different set of problems. It’s more of a slow, creeping issue where excess glucose in the blood leads to inflammation and sluggishness. Instead of a sudden jolt of panic, it often feels like you're trying to walk through mental quicksand.
Because these symptoms are more subtle, they can be harder to connect to your last meal. Keep an eye out for:
- Brain Fog: Having trouble concentrating or feeling mentally "stuck" is a very common sign.
- Agitation and a Short Temper: You might feel restless, on edge, and easily frustrated by things that wouldn't normally bother you.
- Unexplained Fatigue: You just ate, but you feel completely drained and lethargic.
- Increased Thirst: Your body is working overtime to flush out the excess sugar, which can leave you feeling constantly parched.
Key Takeaway: A sugar crash often feels like a sudden, urgent crisis (shaky, anxious), while a sugar high feels more like a slow, draining fog (fatigued, foggy).
Recognizing these distinct patterns is your first step toward getting back in the driver's seat. For a deeper dive into what happens right after a spike, check out our guide on sugar crash symptoms.
To make it even clearer, here’s a quick side-by-side comparison to help you tell the two states apart.
Comparing High vs Low Blood Sugar Symptoms
| Symptom Type | High Blood Sugar (Hyperglycemia) | Low Blood Sugar (Hypoglycemia) |
|---|---|---|
| Emotional | Agitation, anxiety, short temper, difficulty concentrating | Irritability, impatience, anxiety, nervousness, confusion |
| Physical | Fatigue, increased thirst, frequent urination, blurred vision | Shakiness, sweating, dizziness, rapid heartbeat, intense hunger |
By paying attention to these different clues, you can start to understand what your body is telling you and take steps to find your balance.
The Two-Way Street Between Blood Sugar and Mental Health

The link between what you eat and how you feel goes way beyond a simple sugar rush. Think of the connection between blood sugar and mental health as a busy, two-way street—each one has a major impact on the other. When your glucose levels are all over the place, your mood can tank. And when your mind is stressed, managing your blood sugar becomes a whole lot harder.
It’s a frustrating cycle, but understanding it is the first step to breaking free. This is especially true for anyone managing diabetes, insulin resistance, or just dealing with frequent blood sugar mood swings. The daily mental load of managing a health condition can be exhausting, and that emotional toll can turn right around and throw your glucose levels off track.
The Overlap Between Glucose and Mood Disorders
This isn't just a feeling; it's backed by some pretty stark numbers. People with diabetes, for instance, are far more likely to deal with depression and anxiety than the general population.
In fact, about 25% of individuals with diabetes also have a depression diagnosis, and nearly 20% live with anxiety. But you don't need a formal diagnosis to feel this connection. Poor glucose control can make anyone feel more irritable and worried. Diets packed with refined sugars—the kind that cause sharp spikes and even sharper crashes—are notorious for triggering these mood swings. You can dive deeper into the deep link between glucose and depression on Nutrisense.io.
This powerful overlap really drives home the point that managing your blood sugar is also a form of mental self-care. By working to keep your glucose stable, you're giving your brain the solid foundation it needs to stay emotionally balanced.
How Stress and Depression Affect Your Blood Sugar
Now, let's look at the traffic coming from the other direction. When you’re stressed, anxious, or depressed, your body doesn't just register it emotionally—it kicks into physical action. It floods your system with stress hormones like cortisol and adrenaline, which are designed to give you a quick energy boost to handle a perceived threat.
When your mind is under stress, your body prepares for a fight. It releases stored glucose to fuel your muscles, raising your blood sugar levels even if you haven't eaten anything sugary.
This ancient survival response can create real problems for modern-day glucose management.
- Cortisol raises blood sugar: It tells your liver to dump stored glucose into your bloodstream to get you ready for action. If you're chronically stressed, this becomes a constant drip, keeping your blood sugar levels high.
- Adrenaline interferes with insulin: This hormone can make your cells less responsive to insulin, which means glucose has a harder time getting where it needs to go.
- Emotional eating: Let's be honest, stress and low moods often have us reaching for high-sugar, high-fat "comfort foods." These foods then send our blood sugar on yet another rollercoaster.
This feedback loop shows why you can't just focus on one side of the equation. You have to look at the whole picture. Taking care of your mental health through things like mindfulness, therapy, or even simple stress-busting habits is a powerful way to support stable blood sugar. Tackling blood sugar mood swings means looking at both what's on your plate and what's on your mind.
Practical Ways to Keep Your Mood and Energy Steady

Knowing why your blood sugar is sending your mood on a wild ride is the first step. But learning how to stop it is where you really take back the reins.
The great news? You don't need to turn your life upside down. Small, steady adjustments in four key areas—what you eat, how you move, your stress levels, and your sleep—can make a huge difference in your emotional stability and day-to-day energy.
Think of it less as a strict regimen and more as a series of simple course corrections. You’re not banning foods; you’re learning how to combine them for better results. You’re not signing up for grueling workouts; you’re discovering the power of a simple walk. Each step works together to smooth out those glucose peaks and valleys that cause the rollercoaster effect.
Fine-Tune Your Diet for a Stable Mood
What’s on your plate has the most immediate impact on your blood sugar. By making a few smart tweaks, you can slow down how quickly your body absorbs sugar and sidestep the dramatic spikes that always lead to a crash. The aim is to build meals that give you a slow, steady stream of energy.
Here are three simple but incredibly effective principles to start with:
- Build Your Meals Around the Power Trio: For every meal and snack, make sure you have a source of protein, fiber, and healthy fat. These three work together to slow down digestion, meaning glucose trickles into your bloodstream instead of flooding it. For example, trade that apple on its own for an apple with a handful of almonds.
- Make Smart Swaps: You don't have to give up the foods you love. Just swap high-glycemic foods for their lower-glycemic cousins. Think brown rice instead of white, sweet potatoes instead of regular potatoes, and whole-grain bread instead of white.
- Rethink What You Drink: Sugary drinks are like a fast-track to a blood sugar spike. Sodas, juices, and sweetened coffee drinks hit your system almost instantly. Water is always your best bet, but unsweetened tea or sparkling water with a squeeze of lemon are great, too.
Move Your Body to Shift Your Mood
Exercise is a fantastic tool for blood sugar management because it helps your cells become more receptive to insulin. This means your body can actually use the glucose in your blood for energy instead of just letting it hang around causing problems. And no, you don't need to start training for a marathon.
One of the most powerful habits you can build is taking a short walk after you eat. Research has shown that just 15 minutes of walking post-meal can significantly improve your blood sugar levels. This gentle movement encourages your muscles to soak up the glucose from your food, preventing that spike before it even starts.
A post-meal walk acts like a sponge, absorbing excess glucose from your bloodstream before it has a chance to cause a spike and a subsequent emotional crash.
Manage Your Stress to Manage Your Sugar
Stress is more than just a feeling—it sets off a powerful physical chain reaction. When you’re stressed out, your body releases hormones like cortisol, which basically tells your liver to release a bunch of stored sugar into your bloodstream. It’s an ancient "fight or flight" response, but in our modern lives, it just leads to chronically high blood sugar.
Finding healthy outlets for stress isn't just a good idea; it's a must for stable moods.
- Mindfulness and Deep Breathing: Taking even five minutes for quiet meditation or deep breathing exercises can lower your cortisol levels.
- A Consistent Routine: Simply sticking to a predictable schedule for meals and sleep can lower your body's overall stress burden.
- Get Lost in a Hobby: Making time for things you genuinely enjoy—reading, gardening, listening to music—is a proven way to unwind.
Learning to manage your blood sugar is a huge step toward mastering emotional regulation and feeling more in control of your life.
Prioritize Sleep for a Better Insulin Response
Sleep is your body's nightly repair crew, and it’s absolutely critical for how your body handles blood sugar. A lack of quality sleep can make your cells more resistant to insulin the very next day. One study even found that a single rough night is enough to reduce your insulin sensitivity.
Try to get 7-9 hours of quality sleep each night. To get there, you can improve your sleep hygiene:
- Stick to a schedule. Go to bed and wake up around the same time every day, even on the weekends.
- Wind down before bed. Create a relaxing routine, like reading a book (a real one, not on a screen!) or taking a warm bath.
- Ditch the screens. The blue light from phones, tablets, and TVs can mess with your sleep hormones. Try to put them away at least an hour before you plan to sleep.
By focusing on these four pillars—diet, exercise, stress, and sleep—you’re building a solid foundation for stable blood sugar. And with that comes a much more balanced, predictable, and positive mood.
Got Questions About Blood Sugar and Mood? We Have Answers.
It's totally normal to have questions when you start connecting the dots between what you eat and how you feel. Let's clear up a few common ones so you can feel more in control.
How Quickly Can My Mood Improve?
You might be surprised by how fast you can feel a difference. While creating lasting stability is a marathon, not a sprint, many people notice a real shift in their energy and emotional state within just a few days of changing how they eat.
Once you start focusing on meals rich in protein, fiber, and healthy fats, you'll avoid those jarring glucose spikes and crashes that often leave you feeling irritable or anxious. One of the first things you'll likely notice is that the dreaded afternoon slump starts to disappear, replaced by a more consistent and stable mood all day long.
Which Foods Are the Worst Offenders?
Everyone’s body is a little different, but some foods are well-known for sending your blood sugar on a rollercoaster ride, taking your mood right along with it. The main culprits are usually things loaded with refined carbs and added sugars, without any fiber or protein to pump the brakes on absorption.
Keep an eye out for these common triggers:
- Sugary Drinks: Soda, sweetened teas, and even fruit juices are like a direct sugar injection into your bloodstream.
- White Grains: Think white bread, pasta, and rice. They’ve been stripped of their natural fiber, so your body digests them almost instantly.
- Sweet Snacks: Candy, pastries, and cookies give you that quick, feel-good rush, but it’s always followed by a pretty miserable crash.
When Is It Time to See a Doctor?
Making smarter food and lifestyle choices is a huge step, but it’s not a replacement for professional medical advice. You should definitely talk to your doctor if you're experiencing any of the following.
If your mood swings feel severe, happen all the time, or are getting in the way of your job, relationships, or just daily life, it's time to get professional help. A doctor can rule out other underlying issues and help you create a plan that's both safe and effective.
You should also book an appointment if you think you might have a condition like insulin resistance, prediabetes, or diabetes. A doctor can run the right tests and get you on the right path. Never hesitate to reach out when things feel like they're too much to handle on your own.
The connection between how our bodies process sugar and our mental state is undeniable. A global survey found that a staggering 77% of people with diabetes also struggle with their mental health, and about 40% of people with mood disorders show signs of insulin resistance. It's a two-way street, which is why taking care of your physical health is so crucial for your mind. You can learn more about the hidden burden of diabetes on IDF.org.