What Causes Reactive Hypoglycemia and How to Manage It
Ever felt shaky, weak, and utterly drained a few hours after a meal? That sudden crash could be reactive hypoglycemia. It's not a disease in itself, but rather a flashing warning light that your body’s blood sugar regulation is out of whack.
The core issue is an overly aggressive insulin response. Your body essentially overreacts to the food you ate, sending your blood sugar plummeting below normal levels. It's this "reaction" that brings on those unpleasant symptoms.
Untangling the Triggers Behind Your Blood Sugar Crash
Imagine your body’s insulin system is like an overzealous thermostat. When you eat—especially a meal high in sugar or refined carbs—your blood sugar rises. In response, this "thermostat" doesn't just turn on the AC; it blasts it on full, overcorrecting and making the room far too cold.
This is exactly what happens with your blood sugar. The insulin surge is so powerful that it pushes your glucose levels too low, leading to that post-meal crash. While the food you ate is the immediate trigger, the real problem is your body's flawed hormonal response to it.
Distinguishing Triggers from Underlying Causes
To get a handle on this, it's crucial to separate the immediate dietary triggers from the deeper, physiological reasons for the overcorrection.
- Immediate Triggers: Think of things that cause a rapid blood sugar spike. Meals loaded with refined carbohydrates and simple sugars—like soda, white bread, candy, or pasta—are common culprits. They provoke that exaggerated insulin release.
- Underlying Causes: This is the why behind your body's overreaction. It could be early-stage insulin resistance, hormonal imbalances, or even anatomical changes from certain surgeries like gastric bypass.
The central problem in reactive hypoglycemia is a mismatch of timing and quantity. Your body either releases way too much insulin, or it releases it at the wrong time, causing a blood sugar "crash" instead of a gentle return to normal.
For a clearer picture, let's break down the primary causes in a quick summary.
Primary Causes of Reactive Hypoglycemia at a Glance
This table simplifies the main factors that can lead to those post-meal blood sugar crashes, giving you a quick reference for the common culprits.
| Causal Factor | Brief Explanation | Common Examples |
|---|---|---|
| Dietary Choices | Meals high in simple sugars and refined carbs cause a rapid glucose spike, prompting an excessive insulin release. | Sugary drinks, white bread, sweets, processed foods. |
| Insulin Resistance | The body's cells don't respond well to insulin, causing the pancreas to overcompensate by producing more. | Early stages of prediabetes or type 2 diabetes. |
| Hormonal Imbalances | Other hormones, like cortisol and glucagon, that help regulate blood sugar are not functioning correctly. | Adrenal fatigue, thyroid issues. |
| Surgical Procedures | Surgeries affecting the digestive system can alter how food is processed, leading to rapid glucose absorption. | Gastric bypass, stomach surgery. |
Understanding these distinctions is the first step toward managing the condition. It separates the what (the food) from the why (the underlying imbalance).
To dig deeper into your own body's unique metabolic response, exploring options like metabolic stress testing can provide incredibly valuable insights. With this foundation, we can now dive into the more complex mechanisms at play.
The Hormonal Rollercoaster Behind Blood Sugar Crashes
To really get what causes reactive hypoglycemia, we have to look at the hormones that manage your body's fuel. Picture your blood sugar regulation system as a finely tuned seesaw. On one side, you have insulin, the hormone that lowers blood sugar. On the other, you have glucagon, which raises it. When everything is working right, these two work in harmony to keep the seesaw perfectly level.
But with reactive hypoglycemia, that delicate balance gets thrown way off. After you eat—especially something loaded with simple carbs—the insulin side of the seesaw doesn't just gently lower. It slams down with way too much force. This overcorrection is what sends your blood sugar levels plummeting and triggers those awful post-meal symptoms.
This infographic breaks down the basic flow of what’s happening inside your body.
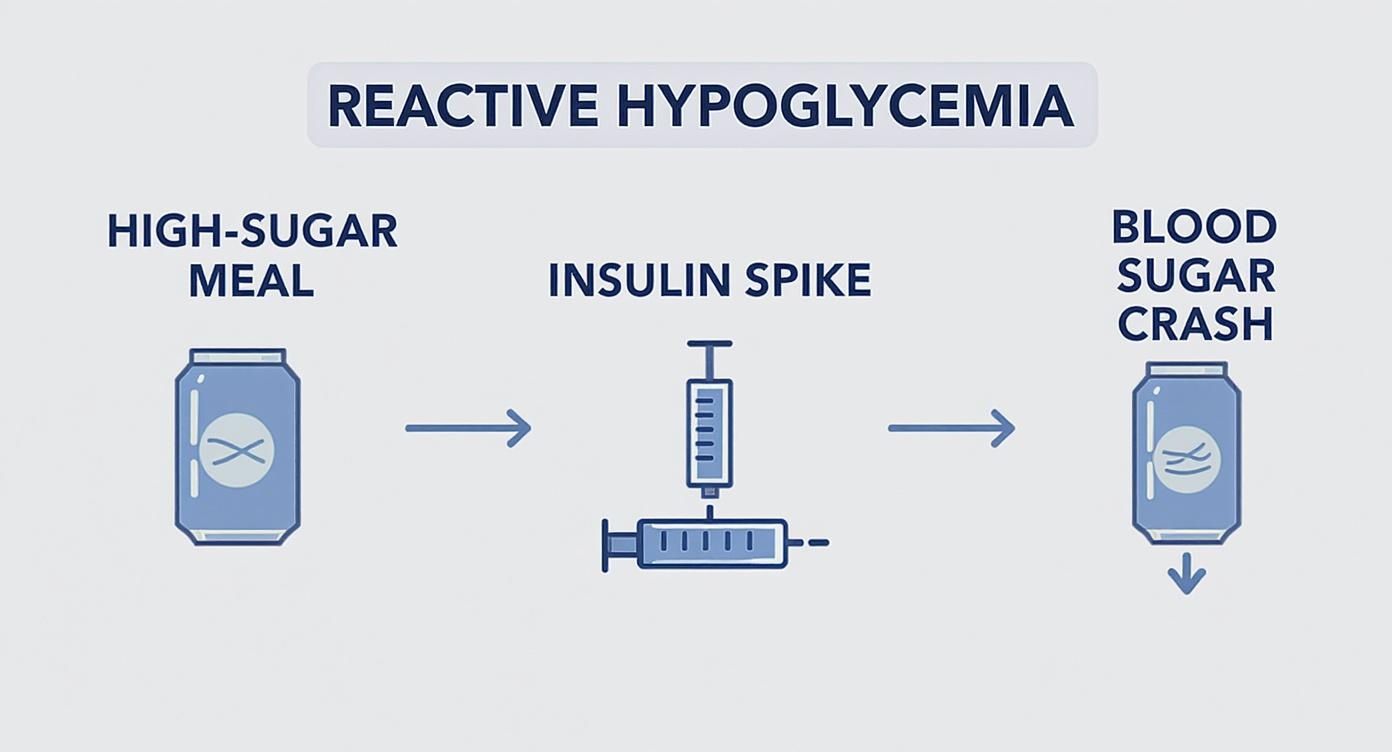
As you can see, it starts with a high-sugar meal, which kicks off a massive insulin spike. That spike is what leads directly to the subsequent blood sugar crash.
The Problem of a Mismatched Insulin Response
At its heart, the problem comes down to bad timing and a massive overreaction. Instead of a smooth, measured insulin release that matches the sugar coming in from your food, your body's response is completely out of sync. This usually unfolds in two distinct, problematic phases.
First, your body might have a delayed or weak insulin release right after you start eating. This allows blood sugar to climb higher and faster than it normally would. Seeing this alarming spike, your pancreas panics and unleashes a huge, exaggerated second wave of insulin to try and fix the problem.
This flood of insulin is what aggressively pulls way too much sugar out of your bloodstream, causing your glucose to crash 2 to 5 hours after a meal. This is the exact biological event that triggers the classic symptoms of reactive hypoglycemia.
In simple terms, your body’s response is too little, too late… and then way too much. This hormonal miscalculation is a huge reason why some people are so prone to these energy crashes. For a deeper dive, you can learn more about the science behind these delayed insulin responses and their impact.
Why Does This Overreaction Happen?
So, what causes this hormonal communication breakdown? Several factors can be at play. For some people, it's an early warning sign of insulin resistance. This is a condition where your body's cells start ignoring insulin's signals, forcing the pancreas to pump out more and more of it just to get the same job done.
This hormonal rollercoaster is also heavily influenced by what you eat. A meal packed with refined carbs and sugar is like pouring gasoline on a fire—it provokes a much more dramatic insulin surge than a balanced meal with protein, fiber, and healthy fats. To see how different foods impact this process, take a look at our guide on what causes insulin spikes.
Ultimately, the hormonal chaos behind reactive hypoglycemia points to a fundamental communication breakdown in your metabolic system. This sets the perfect stage for the dietary triggers we're about to explore.
How Your Diet Can Trigger a Hypoglycemic Reaction
While hormones can set the stage for a blood sugar crash, it's often your plate that plays the starring role. The food you eat has the power to either keep your energy steady or send you on a wild rollercoaster ride. Figuring out which foods are your allies is the first step to heading off a hypoglycemic reaction.
Think of it this way: eating simple sugars and refined carbs is like pouring gasoline on a fire. Sugary sodas, white bread, pastries, and candy hit your system fast, flooding your bloodstream with glucose. This sudden, dramatic spike forces your body to release a huge wave of insulin to deal with it, which leads directly to that infamous crash a couple of hours later.
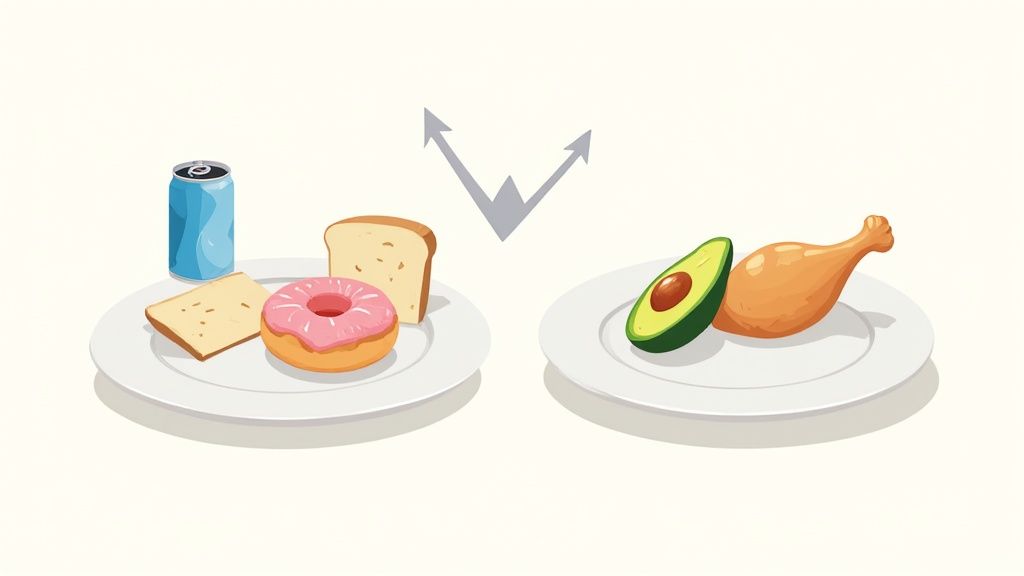
This rapid spike-and-crash cycle is the classic trigger for reactive hypoglycemia. Your body, in its haste, releases too much insulin and overcorrects, clearing way too much sugar from your blood. The result? You're left feeling shaky, weak, and mentally foggy.
High-Glycemic vs. Low-Glycemic Foods
We can measure how quickly a food raises your blood sugar using something called the glycemic index (GI). High-GI foods are the main culprits to watch out for.
- High-GI Foods: These are the "gasoline" foods. They break down in a flash, causing that big blood sugar surge. Think white rice, potatoes, sugary breakfast cereals, and most packaged snacks.
- Low-GI Foods: These are more like slow-burning logs, giving you steady, sustained energy. Foods that are high in fiber, protein, and healthy fats—like whole grains, beans, vegetables, and nuts—are in this camp.
By sticking with low-glycemic foods, you give your body a gentle, steady stream of fuel. This avoids the initial glucose spike that signals an over-the-top insulin release, stopping a hypoglycemic reaction before it even begins.
Taking a moment to understand what the glycemic index is can be a total game-changer. It gives you the knowledge to build meals that support your body instead of working against it.
Building a Stabilizing Plate
The key to preventing diet-induced reactions isn't about ditching carbs altogether. It's about picking the right ones and, just as importantly, balancing them. The goal is to slow down digestion so that glucose is released into your bloodstream gradually.
Here’s a simple rule to live by: never eat a carbohydrate alone. Always pair it with some protein or healthy fat. For example, instead of eating an apple by itself, have it with a small handful of almonds. Instead of plain toast, try whole-wheat toast topped with avocado and an egg. This simple trick softens the glycemic impact and keeps you feeling full and stable for hours.
To make this easier, here's a quick cheat sheet for making smarter food swaps.
Trigger Foods vs. Stabilizing Foods for Reactive Hypoglycemia
This table compares common foods that can trigger a hypoglycemic episode with healthier alternatives that help stabilize blood sugar levels.
| Food Category | Potential Trigger Foods (High Glycemic) | Stabilizing Alternatives (Low Glycemic) |
|---|---|---|
| Grains | White bread, white rice, sugary cereals | Whole-wheat bread, brown rice, quinoa, oats |
| Snacks | Candy, cookies, potato chips, pretzels | Nuts, seeds, Greek yogurt, veggie sticks with hummus |
| Beverages | Soda, fruit juice, sweetened iced tea | Water, unsweetened herbal tea, black coffee |
| Fruits | Watermelon, pineapple (in large amounts) | Berries, apples, pears, cherries |
Making these simple swaps can have a massive impact on your energy levels and overall well-being, helping you avoid the peaks and valleys of a blood sugar rollercoaster.
The Link Between Bariatric Surgery and Hypoglycemia
While diet and hormones are common culprits, one of the most significant—and often challenging—causes of reactive hypoglycemia is bariatric surgery. Procedures like the Roux-en-Y gastric bypass fundamentally change the plumbing of your digestive system, creating a much faster route for food to travel.
Think of your normal digestive tract as a long, winding road with speed bumps that ensure food is processed slowly. Bariatric surgery essentially builds a high-speed expressway, allowing food to bypass large sections of the stomach and duodenum.
This food now "dumps" into the small intestine almost immediately after you eat. Your system isn't prepared for this sudden arrival and sends out a five-alarm signal by releasing a flood of hormones, especially one called GLP-1 (glucagon-like peptide-1).
The GLP-1 and Insulin Overreaction
GLP-1 is the hormone that shouts at your pancreas to release insulin. After gastric bypass, the massive surge of GLP-1 triggers an equally massive, over-the-top insulin response—far more than the meal actually calls for.
This exaggerated insulin release goes into overdrive, aggressively pulling sugar out of your bloodstream. The result is a sharp, dramatic drop in blood sugar, typically hitting 90 to 180 minutes after a meal. This is a well-known complication of gastric bypass surgery, where the body's natural response becomes dangerously amplified. You can read more about the mechanisms of post-bariatric hypoglycemia to understand the process in detail.
Why the Body’s Safety Net Fails
Normally, if your blood sugar drops too low, your body has a built-in safety net. A hormone called glucagon steps in, telling your liver to release its stored glucose to bring your levels back up.
Here’s the problem: after gastric bypass, this glucagon response is often weakened or doesn't happen at all.
Without the glucagon safety net, your body has no way to fight back against the massive insulin surge. This is what makes post-bariatric hypoglycemia so severe and difficult to manage.
This perfect storm of rapid food dumping, an exaggerated GLP-1 and insulin response, and a failed glucagon safety system creates a unique and serious condition. It's a direct result of changing your anatomy, which in turn throws the body's carefully tuned hormonal orchestra into chaos.
Underlying Conditions That Increase Your Risk
Sometimes, that post-meal crash isn't just about what you ate. It can be a red flag that your body is wrestling with a deeper metabolic issue. While a sugar-heavy meal can trigger a blood sugar dip in just about anyone, certain underlying conditions can make you much more vulnerable to these energy nosedives by throwing your body's delicate hormonal balance out of whack.
If you’re consistently feeling drained and shaky after eating, it could be your body’s early warning system trying to get your attention. This blood sugar rollercoaster is often one of the first clues that something is off with how your system is handling glucose and insulin.
Insulin Resistance and Prediabetes
One of the biggest culprits behind reactive hypoglycemia is insulin resistance. Imagine insulin as the key that unlocks your cells to let glucose in for energy. When you have insulin resistance, the locks on your cells get a bit "rusty," making it harder for the key to work.
To compensate, your pancreas goes into overdrive, pumping out extra insulin to force those cell doors open. This initial overproduction is what leads to that massive insulin surge after a meal, which then causes your blood sugar to plummet a couple of hours later. In many cases, reactive hypoglycemia is one of the very first signs you’re on the path toward prediabetes or type 2 diabetes.
Figuring out if you have these metabolic imbalances is a huge step toward prevention. Knowing how to check for insulin resistance can be a game-changer, helping you catch problems before they get more serious.
Polycystic Ovary Syndrome and Hormonal Imbalances
Some people are simply at a higher risk, especially women with Polycystic Ovary Syndrome (PCOS). PCOS is a hormonal disorder that goes hand-in-hand with insulin resistance, creating the perfect storm for the kind of dramatic insulin overreaction that causes blood sugar to crash.
The hormonal chaos of PCOS directly messes with your body's ability to regulate glucose. This puts your metabolism under constant stress, forcing the pancreas to work much harder than it should.
The research really drives this point home. One Danish study revealed that a staggering 17% of women with PCOS dealt with reactive hypoglycemia, while none of the women in the control group did. That stark contrast shows just how much the impaired insulin function in PCOS makes you susceptible to these post-meal crashes. You can read the full research about these findings for a deeper dive into the connection.
Other factors can also stack the deck against you, including:
- A Family History of Diabetes: Your genes can play a big role in how well your body manages insulin.
- Adrenal or Pituitary Gland Issues: These glands are responsible for hormones that help keep insulin in check. If they aren't working properly, it can disrupt your body's natural safety net against low blood sugar.
It’s all about connecting the dots. Your after-meal symptoms might not be a random occurrence but a clear sign pointing to a bigger health picture that deserves a closer look.
Practical Steps to Manage and Prevent Episodes
Knowing what causes reactive hypoglycemia is half the battle. The other half is taking action to prevent it, and thankfully, you have a lot of control here. Making some smart, sustainable lifestyle changes can dramatically reduce those awful post-meal energy crashes. It all starts with getting to know your body's unique responses.
A great first step is to start a simple food-and-symptom journal. Seriously, this can be a game-changer. Just jot down what you eat and how you feel two to four hours later. This helps you connect the dots and identify your personal triggers. Plus, having this log makes conversations with your doctor far more productive if you decide to seek a formal diagnosis, which might involve an Oral Glucose Tolerance Test (OGTT).
Smart Strategies for Stable Blood Sugar
Keeping your blood sugar stable isn't about extreme dieting. It's about being more strategic with how you eat and move to avoid the big glucose spikes that trigger that over-the-top insulin response.
Here are three core strategies that really work:
- Eat Smaller, More Frequent Meals: Instead of three large meals a day, aim for five or six smaller ones. This gives your body a slow, steady supply of energy and prevents the sudden sugar rushes that lead to a crash.
- Pair Your Nutrients Wisely: This is a golden rule: never eat carbs by themselves. Always pair them with a good source of protein and healthy fat. This simple habit slows down how quickly your body absorbs the sugar, leading to a much gentler rise and fall in your glucose levels.
- Incorporate Gentle Movement: You don't need an intense workout. A simple 10-minute walk after a meal can do wonders. Moving helps your muscles pull glucose directly from your bloodstream for energy, meaning your pancreas doesn't have to pump out as much insulin.
The real secret here is consistency. When you make these small adjustments part of your daily routine, you're essentially retraining your body’s metabolic response. You shift from a cycle of sugar highs and lows to one of stable, predictable energy.
Putting these habits into practice is the most effective way to manage your symptoms and stop future episodes in their tracks. For an even deeper dive into what to eat and when, check out these actionable tips to stabilize blood sugar levels.
Got Questions About Reactive Hypoglycemia? Let's Clear Things Up.
Trying to figure out reactive hypoglycemia can feel confusing, and it's natural to have questions. Here are some straightforward answers to the things people ask most often.
Is Reactive Hypoglycemia a Sign of Diabetes?
It can be a red flag, but it’s not a direct diagnosis of diabetes. Think of it more like your body's check-engine light coming on.
Reactive hypoglycemia often points to insulin resistance, which is the very same issue that can eventually lead to prediabetes and type 2 diabetes. So, while it's not diabetes itself, it’s definitely a sign that your body is struggling to manage blood sugar correctly. If you're experiencing symptoms, getting checked out by a doctor is the best move you can make.
Can I Have Reactive Hypoglycemia If I'm Not Overweight?
Absolutely. It’s a common misconception that blood sugar issues only affect people who are overweight.
While carrying extra weight is a risk factor for insulin resistance, reactive hypoglycemia can happen to anyone, regardless of their body size. The real issue is how your body responds to the food you eat, and that can be influenced by genetics, hormonal conditions like PCOS, or other metabolic factors that have nothing to do with your weight.
The Bottom Line: Reactive hypoglycemia is about how your metabolism functions, not how much you weigh. It's an internal response, not an external one.
How Is This Different from "Regular" Hypoglycemia?
The key difference all comes down to timing and triggers.
Fasting hypoglycemia is what most people think of—your blood sugar drops because you haven’t eaten in a while and your body is running on empty.
Reactive hypoglycemia, on the other hand, is the opposite. It happens because you ate, usually within two to five hours of a meal. Your body releases too much insulin in response to the food, causing your blood sugar to crash later. It’s a reaction, not a lack of fuel.