What Is Fructose Intolerance Explained
When you hear the term fructose intolerance, you might picture someone who just gets a bit of a stomach ache after eating an apple. While that can be true, it’s only a small part of a much bigger story. The reality is that this term covers two very different conditions, and understanding which is which is absolutely key.
Fructose is a simple sugar found naturally in fruits and vegetables, and it's also a major ingredient in sweeteners like high-fructose corn syrup. For most of us, our bodies handle it without a second thought. But for some, eating fructose kicks off a chain reaction of uncomfortable, and in some cases, dangerous symptoms.
The Two Faces of Fructose Intolerance
Think of it this way: imagine two different reasons why a package doesn't get delivered. One reason might be a simple traffic jam slowing down the delivery truck—an annoying but manageable problem. The other could be that the destination address doesn't exist, causing a much more serious breakdown in the system. Fructose intolerance works in a similar way.
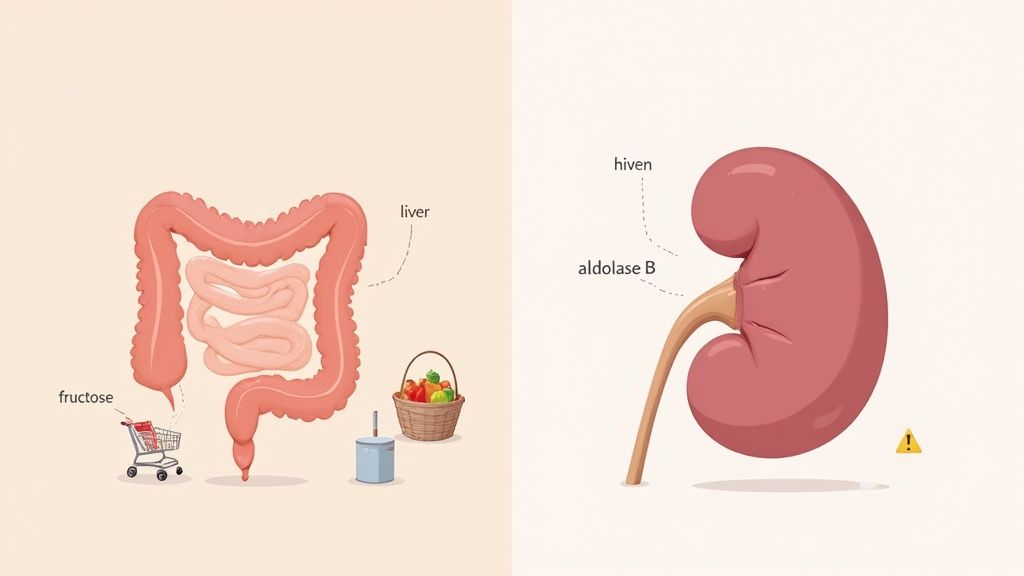
The first type, and by far the most common, is fructose malabsorption. This is the "traffic jam" scenario. It’s a digestive issue where the cells in your small intestine just can't absorb fructose efficiently. That undigested sugar then moves into the large intestine, where gut bacteria have a feast. This fermentation process creates gas, leading to bloating, cramping, and diarrhea.
The second, much rarer condition is hereditary fructose intolerance (HFI). This is a serious genetic disorder—the "non-existent address." People with HFI are born without a crucial enzyme, aldolase B, which is needed to break down fructose. When they eat it, toxic substances build up in their liver and kidneys, causing severe health problems.
While HFI is quite rare, affecting around 1 in 20,000 to 30,000 people, fructose malabsorption is surprisingly common. Some studies suggest it affects up to 40% of people in Western countries, as highlighted in insights from Frusano.com.
The key takeaway is simple: Malabsorption is a transportation problem in the gut, whereas HFI is a metabolic defect in the liver. Differentiating between them is the first and most critical step toward proper management.
The flowchart below breaks down how these two distinct paths unfold in the body.
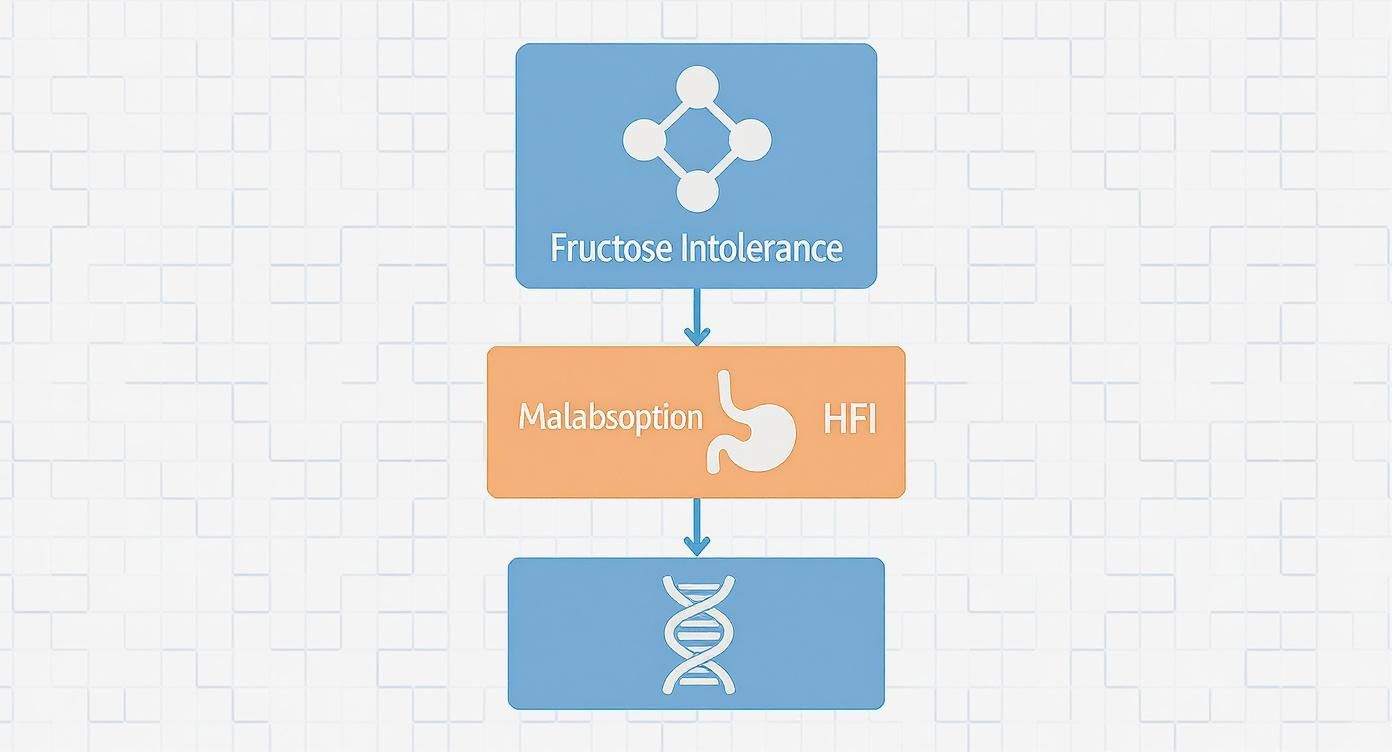
This visual helps clarify the root cause of each condition—one being a digestive hiccup and the other a serious genetic issue. Knowing which path you might be on is crucial because the way we diagnose and manage them couldn't be more different.
To make the distinction even clearer, let's compare them side-by-side.
Fructose Malabsorption vs Hereditary Fructose Intolerance (HFI) at a Glance
| Feature | Fructose Malabsorption (Digestive Disorder) | Hereditary Fructose Intolerance (Genetic Disorder) |
|---|---|---|
| Cause | The small intestine cannot absorb fructose properly. | Born without the enzyme (aldolase B) needed to break down fructose. |
| Prevalence | Common; affects up to 40% of the population in some regions. | Rare; affects 1 in 20,000 to 30,000 people. |
| Onset | Can develop at any age, often in adulthood. | Symptoms begin in infancy, usually when fruits or formula with fructose are introduced. |
| Symptoms | Digestive discomfort: bloating, gas, cramps, diarrhea. | Severe: nausea, vomiting, low blood sugar, liver and kidney damage. Can be life-threatening. |
| Severity | Uncomfortable and disruptive, but not life-threatening. | Very serious and requires lifelong, strict avoidance of all fructose and sucrose. |
As you can see, while both conditions revolve around fructose, their impact on your health is worlds apart. Now, let’s dive into how you can figure out what’s really going on.
Understanding the Two Types of Fructose Intolerance
When you hear "fructose intolerance," it's easy to picture a single, straightforward condition. But the reality is that this term covers two very different health issues that just happen to share the same trigger: fructose. Knowing which is which is the crucial first step to figuring out what’s going on in your body and how to manage it.
One is a common digestive issue, while the other is a serious genetic disorder. Let's walk through each one to make the difference crystal clear.
Fructose Malabsorption: The Digestive Overload
Fructose malabsorption is, by a long shot, the more common of the two. Think of your small intestine as a tiny tollbooth on a major highway. It has a limited number of lanes and can only process so many cars (or fructose molecules) at once.
If you only eat a little fructose, like a handful of blueberries, the tollbooth handles the traffic just fine. The sugar gets absorbed into your bloodstream to be used for energy. But if you down a huge glass of apple juice or a dessert loaded with high-fructose corn syrup, you create a massive traffic jam. The system gets completely overwhelmed.
All that extra, unabsorbed fructose has to go somewhere, so it continues its journey down to the large intestine. Down there, it becomes an all-you-can-eat buffet for your gut bacteria. As they start feasting on the sugar, they produce a ton of gas and draw water into the colon.
This fermentation party is what causes those classic, uncomfortable symptoms:
- Bloating and Gas: All that gas produced by the bacteria has to go somewhere.
- Abdominal Pain: The intestinal walls stretch from the excess gas and water, leading to cramps and pain.
- Diarrhea: The extra water in the colon creates loose, urgent bowel movements.
The key thing to remember here is that fructose malabsorption is a dose-dependent problem. One person might feel fine after eating an orange but get hit with symptoms after drinking a soda. It all comes down to how much fructose you eat and what your personal absorption limit is.
Hereditary Fructose Intolerance: The Metabolic Breakdown
Now, let's switch gears to the other condition, hereditary fructose intolerance (HFI). This is a whole different ballgame. We’re not talking about a digestive traffic jam anymore; this is a fundamental breakdown in your body's metabolic engine.
HFI is a rare genetic disorder. People with HFI are born missing a crucial liver enzyme called aldolase B. This enzyme’s one and only job is to break down fructose after it’s been absorbed. Without it, the whole process grinds to a halt.
When someone with HFI eats fructose, its byproducts build up in the body, mostly in the liver and kidneys. These substances are toxic. They actively block the body from making glucose (its main fuel) and keeping blood sugar levels stable.
HFI is far more serious than just an upset stomach. Consuming even a tiny bit of fructose can lead to dangerous, system-wide health complications.
This rare metabolic disorder is caused by inheriting a mutated gene from both parents. It's estimated to affect between 1 in 18,000 to 1 in 60,000 people around the world. You can learn more about the specific genetics of HFI from this helpful MedlinePlus resource.
The symptoms of HFI are worlds apart from malabsorption and usually show up in infancy, right when a baby is introduced to foods containing fructose or sucrose.
The tell-tale signs of HFI include:
- Severe hypoglycemia (dangerously low blood sugar) after eating fructose
- Vomiting and nausea
- Jaundice (a yellowing of the skin and eyes)
- Lethargy and poor feeding in babies
- Over time, it can lead to severe liver and kidney damage
Because the risks are so high, anyone with HFI must follow a strict, lifelong diet that completely eliminates fructose, sucrose (which is half fructose), and sorbitol. It's the only way to prevent organ damage and life-threatening emergencies. Grasping this distinction isn’t just interesting—it’s absolutely essential for staying safe and getting the right medical care.
Recognizing the Symptoms of Fructose Intolerance
The first step to understanding fructose intolerance is learning to read the signs your body is sending. These symptoms aren't random; they're direct clues telling a story about how your body is struggling with fructose. But that story can have two completely different plots, depending on whether you're dealing with a simple digestive traffic jam or a serious metabolic defect.
The symptoms of fructose malabsorption and hereditary fructose intolerance (HFI) are worlds apart. One set is deeply uncomfortable and disruptive, while the other is a series of red flags signaling a medical emergency.

Let's break down the distinct signs for each condition so you can get a clearer picture of what might be happening.
Symptoms of Fructose Malabsorption: The Digestive Distress Signals
When you have fructose malabsorption, your symptoms are almost entirely centered around your digestive system. Think of it as a localized protest happening right in your gut. This reaction kicks off when undigested fructose makes it to the large intestine, where gut bacteria have a feast. They ferment it, producing gas and pulling a lot of water into the colon.
The result? A collection of familiar and very unpleasant gastrointestinal issues.
These symptoms usually show up anywhere from 30 minutes to a few hours after you've eaten something high in fructose. How bad they get often depends on just how much fructose you ate.
Common signs of fructose malabsorption include:
- Bloating and Gas: This is probably the most common complaint. The fermentation process literally pumps your intestines full of gas, leaving you with that swollen, tight feeling.
- Abdominal Pain and Cramping: All that extra gas and water stretches the intestinal walls, which can cause real discomfort, from dull aches to sharp, stabbing cramps.
- Diarrhea: The excess water that gets pulled into the colon leads to loose, watery, and often urgent trips to the bathroom.
- Nausea: While not as frequent as bloating or diarrhea, some people definitely feel queasy after a fructose-heavy meal.
It's crucial to understand that these symptoms, while miserable, are not dangerous. However, they can absolutely wreck your quality of life. The constant discomfort and unpredictability can make everything from a dinner out to a normal workday feel like a challenge.
For example, you might feel perfectly fine after a handful of strawberries but end up severely bloated from a large glass of apple juice. This is why tracking your reactions is so important for figuring out your personal tolerance level. Using a tool like the StopSugar app to log your meals and symptoms can be a game-changer, helping you connect the dots between what you eat and how you feel.
Symptoms of Hereditary Fructose Intolerance: The Systemic Red Flags
Hereditary Fructose Intolerance (HFI) paints a completely different and far more alarming picture. Because HFI is a genetic metabolic disorder, the symptoms extend well beyond the gut. They are systemic, severe, and a sign that the body is being poisoned from the inside.
These symptoms almost always appear for the first time in infancy. It typically happens right when a baby is weaned from breast milk and introduced to things like formula, fruits, or juices that contain fructose or sucrose.
The signs of HFI are immediate and serious:
- Severe Hypoglycemia: After having fructose, a child with HFI will experience a dangerous plunge in blood sugar. This can look like shakiness, sweating, extreme irritability, or even seizures.
- Vomiting and Nausea: The body’s first line of defense against the toxic buildup is often to try and get the food out, leading to forceful vomiting.
- Jaundice: A yellowing of the skin and the whites of the eyes is a classic sign that the liver is under serious stress and isn't working correctly.
- Aversion to Sweets: Toddlers and young children with undiagnosed HFI often develop a powerful, instinctual dislike for anything sweet. It's their body’s own built-in protection mechanism.
If fructose keeps getting into their system, the long-term consequences are dire, potentially leading to liver failure, kidney damage, and even a coma. Unlike fructose malabsorption, HFI is not about how much you eat—even tiny amounts of fructose are toxic. This makes getting a diagnosis and starting a complete, lifelong avoidance of fructose, sucrose, and sorbitol absolutely critical for survival and a healthy life.
How Doctors Diagnose Fructose Intolerance
If you think fructose might be the source of your troubles, the only way to know for sure is to see a doctor. Trying to figure this out on your own can be confusing, and if Hereditary Fructose Intolerance (HFI) is the culprit, self-diagnosing can be downright dangerous.
The diagnostic path for the two main types of fructose intolerance—malabsorption and HFI—are worlds apart. A doctor will start by talking through your symptoms, your family's medical history, and what you typically eat. This conversation is key, as it helps them decide which condition is more likely and points them toward the right (and safe) way to test for it.
Diagnosing Fructose Malabsorption
When it comes to the more common digestive issue, fructose malabsorption, the go-to diagnostic tool is a simple, non-invasive procedure called the Hydrogen Breath Test. It’s a straightforward way to see exactly how your body is handling fructose.
Here’s a quick rundown of what to expect:
- Get a Baseline: First, you’ll blow into a small device to measure the normal amount of hydrogen in your breath.
- Drink the Fructose: Next, you'll drink a solution containing a measured dose of fructose.
- Breathe and Wait: Over the next couple of hours, you'll provide breath samples every 15 to 30 minutes.
So, how does it work? If your small intestine isn't absorbing fructose properly, that sugar continues its journey down to your colon. There, the bacteria in your gut have a feast, fermenting the fructose and producing hydrogen gas in the process. This gas gets absorbed into your bloodstream, makes its way to your lungs, and you breathe it out. A significant jump in your breath's hydrogen levels is a clear sign of fructose malabsorption.
Diagnosing Hereditary Fructose Intolerance
Now, if a doctor suspects HFI, the diagnostic playbook changes completely. For safety reasons, the Hydrogen Breath Test is strictly off-limits for anyone who might have this genetic condition. Giving a concentrated fructose drink to someone with HFI could trigger a severe and dangerous reaction.
Critical Safety Note: A breath test must be avoided if HFI is even a remote possibility. The test could lead to a sudden drop in blood sugar (hypoglycemia), vomiting, and potentially severe liver problems.
Instead of testing how the body reacts to fructose, doctors focus on finding the genetic root of the problem.
- Genetic Testing: The most definitive way to diagnose HFI is with a blood test. This test screens your DNA for mutations on the ALDOB gene—the gene responsible for making the enzyme that breaks down fructose. Finding the specific mutation confirms the diagnosis.
- Enzyme Assay: In very rare situations, a doctor might take a small sample of liver tissue (a biopsy) to measure the enzyme's activity directly. However, genetic testing is much more common and far less invasive today.
For people with HFI, eating fructose can cause a dramatic drop in blood sugar. This is a serious issue, and if you're looking into blood sugar problems, you might want to understand more about what causes reactive hypoglycemia in our detailed guide.
Knowing the difference between these diagnostic routes is so important. It helps you have a more informed conversation with your doctor, ask the right questions, and make sure you get the proper tests for your situation. Getting that clarity is the first step toward managing your health safely and feeling like yourself again.
Practical Strategies for Managing Fructose Intolerance
Living well with fructose intolerance isn't about chasing a miracle cure; it's about mastering a new way of eating. The right approach really hinges on which type of intolerance you're dealing with, as the strategies can range from careful moderation to complete avoidance.

Think of it like this: for someone with fructose malabsorption, it's like having sensitive skin. A little sun is fine, but too much leads to a painful burn. It’s all about finding that limit. But for someone with Hereditary Fructose Intolerance (HFI), it’s more like a severe sun allergy—any exposure is harmful. This section will give you actionable advice to help you regain control and feel better, no matter which path you’re on.
The Lifelong Diet for Hereditary Fructose Intolerance
If you have Hereditary Fructose Intolerance (HFI), managing your diet isn't just a good idea—it's a medical necessity. Because the body completely lacks the enzyme to process fructose, even tiny amounts can cause a toxic buildup and lead to severe organ damage. This means a strict, lifelong diet is the only way to stay healthy.
The main goal is to completely eliminate three key sugars:
- Fructose: This simple sugar is found in fruits, honey, and tons of processed foods. It has to go.
- Sucrose: This is just plain old table sugar. It’s made of one part glucose and one part fructose, and when your body digests it, that fructose is released. That makes it just as dangerous.
- Sorbitol: This sugar alcohol, often used as a sweetener, actually converts to fructose inside the body.
For HFI, diet is everything. Sticking to a strict fructose-, sucrose-, and sorbitol-free plan is the only way to prevent progressive damage to the liver and kidneys. The great news? With this careful control, people with HFI can lead full, healthy lives.
Finding Your Limit with Fructose Malabsorption
With fructose malabsorption, your journey is less about total elimination and more about personal discovery. The goal is to figure out your unique tolerance threshold—that sweet spot where you can enjoy some foods without triggering awful symptoms like bloating, gas, and diarrhea.
This process usually kicks off with a structured elimination diet. This gives your gut a much-needed break to calm down and reset. One of the most common and effective ways to do this is with a low-FODMAP diet. FODMAPs are a whole group of poorly absorbed carbs, and fructose is a big one.
The game plan for malabsorption is a two-step dance: first, you eliminate foods to find relief. Then, you reintroduce them to find your personal balance. This approach puts you in the driver's seat, helping you build a sustainable diet that truly works for you.
After an initial elimination phase, which usually lasts 2-6 weeks, you’ll slowly start reintroducing fructose-containing foods. You'll bring them back one at a time, paying close attention to how your body reacts. This helps you pinpoint not just which foods cause trouble, but also how much of them you can handle.
Your Grocery Guide: High and Low Fructose Foods
Navigating the grocery store can feel like a minefield when you're just starting out. To make it a little easier, we’ve put together a handy guide to common foods, broken down by their fructose content.
Common Foods High and Low in Fructose
This table is a great starting point for your shopping trips and meal planning, but remember it's a guide, not a set of absolute rules.
| Food Category | High Fructose (Often Avoided or Limited) | Low Fructose (Generally Safer) |
|---|---|---|
| Fruits | Apples, Pears, Mangoes, Watermelon, Cherries | Berries (Strawberries, Blueberries), Citrus (Oranges, Lemons), Bananas (unripe), Avocado |
| Vegetables | Asparagus, Artichokes, Sugar Snap Peas, Leeks | Carrots, Spinach, Zucchini, Cucumbers, Bell Peppers, Potatoes |
| Sweeteners | High-Fructose Corn Syrup, Honey, Agave Nectar | Glucose, Dextrose, Stevia, Maple Syrup (in moderation) |
| Grains | Wheat-based products (can be high in fructans) | Rice, Oats (certified gluten-free), Quinoa, Corn |
| Dairy | Flavored Yogurts, Sweetened Milk Drinks | Plain Yogurt, Cheese, Unsweetened Milk, Lactose-Free Milk |
For a more exhaustive resource, be sure to check out our complete guide on finding the right low fructose food options for your diet.
Keep in mind that with malabsorption, personal tolerance can vary wildly. A food that one person can't touch might be perfectly fine for you in small amounts. That’s why tracking your own symptoms is so important. Beyond diet alone, looking into other natural approaches for digestive problems can also offer great support for your overall gut health.
Your Fructose Questions, Answered
As we get to the end of our guide, you probably still have a few questions rolling around in your head. That's completely normal. Figuring out fructose intolerance can feel like putting together a puzzle, but getting clear answers is the best way to gain control.
Let's dive into some of the most common questions people ask. We'll break them down with simple, straightforward answers to help you connect the dots.
Can You Develop Fructose Intolerance Later in Life?
This is a great question, and the answer really depends on which type of intolerance we're talking about. The difference between the two conditions is everything here.
Hereditary Fructose Intolerance (HFI) is a genetic condition you’re born with. It’s caused by a faulty gene from both parents, so the enzyme that breaks down fructose has been missing from day one. Symptoms almost always show up in infancy when fructose first enters the diet. So no, you can't suddenly develop HFI as an adult.
Fructose malabsorption, on the other hand, can absolutely show up or get worse later in life. Many people go for years without any real problems. But then something changes—it could be a shift in your gut bacteria, a bout of gastroenteritis, chronic stress, or the development of a condition like Irritable Bowel Syndrome (IBS). These factors can either trigger symptoms or make a mild, unnoticed intolerance much more obvious.
In short: HFI is genetic and present from birth. Malabsorption is a digestive issue that can pop up or worsen at any age, often due to changes in your gut health.
Is Fructose Intolerance the Same as a Fructose Allergy?
It's so easy to mix up "intolerance" and "allergy," but they are fundamentally different things happening inside your body. Getting this right is crucial for understanding your symptoms.
A food intolerance is a digestive problem. With fructose malabsorption, your gut struggles to absorb the sugar, which leads to fermentation, bloating, and gas. With HFI, your body can’t metabolize fructose, causing a toxic buildup. Notice what’s missing? The immune system. It doesn’t get involved at all.
A food allergy is an immune system problem. When you have an allergy, your immune system mistakenly sees a food protein as a threat. It goes on the attack, releasing chemicals like histamine that cause classic allergic reactions.
These reactions look very different from intolerance symptoms and can include:
- Hives, rashes, or itchy skin
- Swelling of the lips, tongue, or throat
- Wheezing or trouble breathing
- In severe cases, a life-threatening reaction called anaphylaxis
True fructose allergies are incredibly rare. When people react to fruit, it's usually an allergy to a specific protein in the fruit itself, not the fructose molecule. If your symptoms are all about digestive distress, you're almost certainly dealing with an intolerance, not an allergy.
What Is the Difference Between Fructose and Glucose?
To really get a handle on fructose intolerance, you need to understand how fructose differs from its cousin, glucose. They’re both simple sugars, but your body treats them in completely different ways. This is why you can feel fine after eating one but terrible after another.
Think of it like this: Glucose is the body's universal fuel. Nearly every cell can grab it directly from your bloodstream and use it for instant energy. It’s simple, efficient, and what your brain and muscles run on.
Fructose, however, is a specialty fuel. It can't be used directly by most of your cells. Instead, it has to be sent to a specific processing plant—your liver. There, the liver converts it into other things, like glucose, stored energy (glycogen), or fat.
This unique metabolic path is the key to fructose intolerance. With malabsorption, the special transporters in your gut that are supposed to grab fructose get overwhelmed. With HFI, the liver’s processing plant is missing a vital piece of machinery (the aldolase B enzyme).
Figuring out the specific sugar content of your food is a game-changer. For a detailed guide, our sugars in fruits chart is a fantastic resource to have on hand when planning your meals. The bottom line is, not all sugars are the same, and knowing the difference is the first step toward feeling your best.