Does sugar cause inflammation: A Quick Guide to Health
Let's cut right to it: yes, eating too much added sugar can absolutely cause inflammation.
Now, it's important to know that not all inflammation is bad. When you get a cut, that temporary redness and swelling is your body's natural, helpful healing response. But the kind of inflammation we're talking about with sugar is different. It’s a low-grade, simmering irritation that sticks around and can quietly contribute to serious health problems down the road.
The Clear Answer on Sugar and Inflammation
To really grasp the connection, think about the two main types of inflammation.
Acute inflammation is your body's first responder. It’s the quick, targeted reaction to an injury or infection—that swelling around a sprained ankle, for example. It’s a sign your immune system is on the job, repairing damage and fighting off germs. This process is short-lived and vital for healing.
On the other hand, a high-sugar diet can fuel chronic inflammation. This is a much sneakier, long-term problem where your body's inflammatory alarm bells are constantly ringing, just at a low volume. Instead of healing you, this persistent state can eventually start damaging healthy cells, tissues, and organs, setting the stage for a host of health issues.
The Evidence Linking Sugar to Inflammation
This isn't just a hunch; the link between sugar and inflammation is backed by solid research. Study after study shows that people who eat a lot of sugar have higher levels of inflammatory markers in their blood—basically, little red flags telling doctors that the body is in a state of chronic irritation.
One compelling study on semi-professional football players drove this point home. Researchers found that the athletes who consumed the most simple sugars had significantly higher levels of an inflammatory marker called hs-CRP. In fact, their levels jumped by as much as 25% compared to the players eating the least amount of sugar. This shows that even in highly active, fit individuals, too much sugar still fuels inflammation. You can dig into the full study about sugar and inflammation in athletes to see the details for yourself.
Sugar's Inflammatory Impact At a Glance
So, how exactly does sugar stir up trouble? To put it simply, it triggers a chain reaction in your body. This table breaks down the core ways sugar drives inflammation, making the connection easy to see.
| Key Area | Summary of Impact | Primary Sugars Involved |
|---|---|---|
| Blood Sugar Spikes | Rapid increases in blood glucose trigger the release of inflammatory messengers. | Glucose, Sucrose (table sugar) |
| Gut Health Disruption | Feeds harmful bacteria, leading to an imbalanced gut that can leak toxins. | All added sugars, especially fructose |
| Liver Stress | Excessive fructose metabolism in the liver can generate inflammatory byproducts. | Fructose, High-Fructose Corn Syrup |
| Cellular Damage | Leads to the formation of harmful compounds called AGEs that promote inflammation. | All simple sugars |
In short, from spiking your blood sugar to stressing your liver and disrupting your gut, sugar hits your body from multiple angles, all of which can crank up the dial on chronic inflammation.
How Sugar Triggers Your Body's Inflammatory Response
So, when people ask, "does sugar really cause inflammation?" the answer is a resounding yes. To see why, we need to peek behind the curtain at what happens inside your body when you eat it. Sugar isn't just empty calories; it kicks off a chain reaction that actively promotes inflammation.
This flowchart lays it out simply: eating sugar leads to inflammation, which in turn raises your risk for a host of health problems.
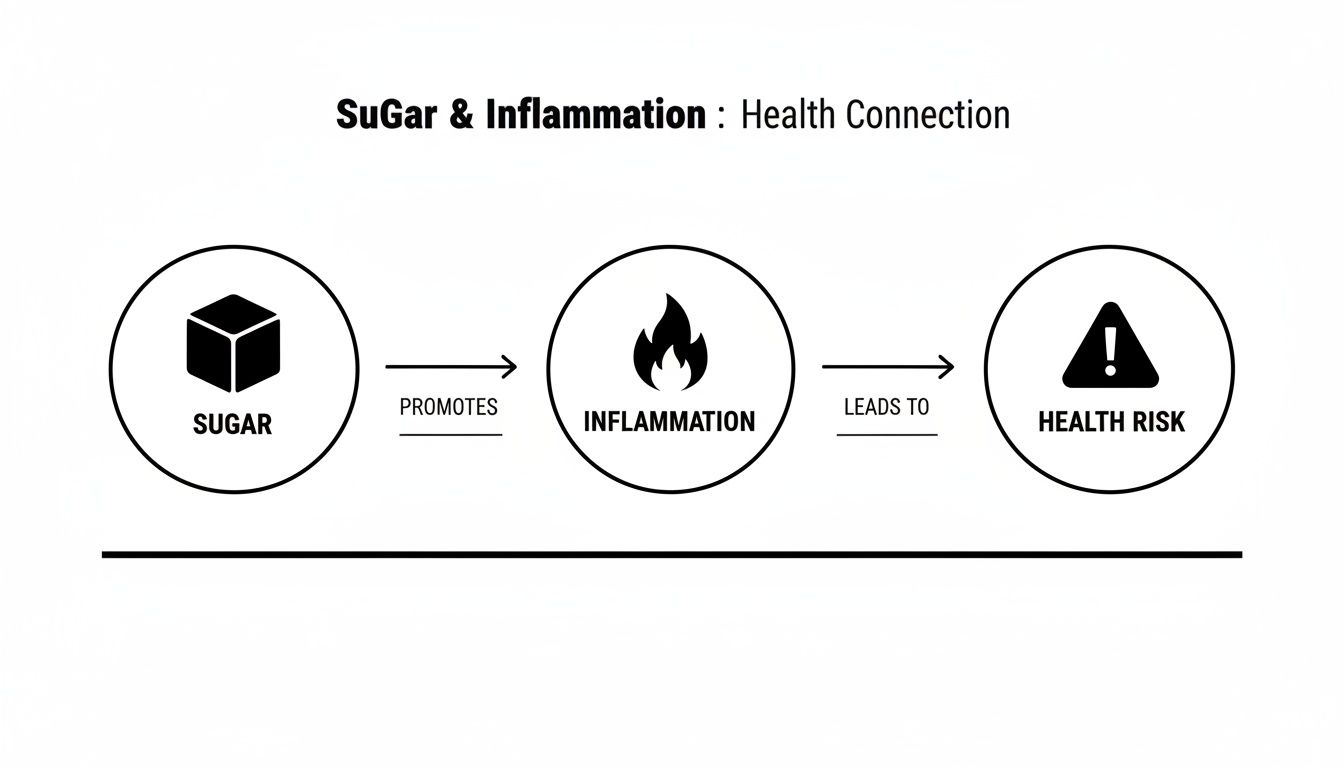
As you can see, sugar isn't just a passive ingredient—it’s an active player that can start a harmful domino effect in your body. Let's break down the three main ways this happens.
The Formation Of Harmful AGEs
One of the biggest culprits is a process called glycation. Picture sugar molecules as sticky little troublemakers floating around in your bloodstream. When they bump into proteins and fats, they latch on, creating damaging new compounds called Advanced Glycation End-products, or AGEs.
Your body doesn't like these AGEs one bit. It sees them as threats, like tiny invaders, and immediately launches an immune response. To fight them off, your system releases inflammatory messengers known as cytokines.
While this is meant to be a protective measure, a diet consistently high in sugar means you're constantly churning out AGEs. This forces your body into a state of chronic, low-grade inflammation—it's always in "attack mode." Think of it like a security alarm that's always buzzing quietly in the background, eventually wearing out the entire system. Over time, this process can make essential proteins, like the collagen in your skin and blood vessels, become stiff and dysfunctional.
The Problem With Insulin Spikes
Whenever you eat sugar, your blood glucose levels go up. Your pancreas then releases insulin, a hormone tasked with moving that glucose out of your blood and into your cells for energy. When everything is in balance, this is a perfectly normal process.
The problem starts when you consume a lot of refined sugars and simple carbs. This causes a massive, rapid surge in blood glucose, forcing your pancreas to work overtime and flood your system with insulin to handle the sugar dump. These sudden insulin spikes are a direct trigger for inflammation.
High levels of insulin can activate pro-inflammatory pathways in the body. The hormone itself can signal fat cells to produce and release inflammatory cytokines, contributing directly to systemic inflammation.
Over time, your cells can start to ignore insulin's constant signals, leading to a condition called insulin resistance. This makes the problem even worse, as your pancreas has to pump out even more insulin to get the job done. It's a vicious cycle of high blood sugar, high insulin, and relentless inflammation. You can dive deeper into this in our guide on what causes insulin spikes.
Disruption Of Your Gut Health
Your gut is home to a massive community of bacteria—some good, some bad. Keeping them in a healthy balance is critical for just about everything, especially keeping inflammation in check. Unfortunately, sugar is the favorite food of the harmful bacteria living in your gut.
When your diet is high in sugar, you're essentially throwing a feast for the bad guys. They multiply and start to overpower the beneficial bacteria. This imbalance, known as gut dysbiosis, creates a chaotic and unhealthy environment in your digestive system.
This leads to a problem often called "leaky gut." The harmful bacteria can damage the intestinal lining, allowing toxins and other particles to leak into your bloodstream where they absolutely do not belong. Your immune system spots these intruders and goes on high alert, launching a powerful inflammatory attack.
Recent research shows just how big of a deal this is. With sugar making up a staggering 17% of the calories in the average American diet, it's constantly fueling this gut imbalance. Studies show this can cause harmful bacteria populations to double, leading to toxins leaking from the gut and increasing inflammatory markers by up to 40%. This constant leakage and the resulting immune firefight are a major driver of the chronic inflammation linked to high sugar intake.
Why The Source of Sugar Matters for Inflammation
When we talk about sugar and inflammation, one thing needs to be crystal clear: not all sugars are the same. Your body's response to the sugar in a juicy apple is worlds apart from how it handles the sugar in a can of soda. It all comes down to the source—where that sugar came from is the single most important factor.
Think of it like fuel for a fire. The sugar in whole fruit is like a slow-burning log, releasing energy steadily over time. In contrast, the processed sugar in a candy bar is like throwing gasoline on the flames—it causes a sudden, explosive reaction. This huge difference lies in how the sugar is "packaged."

Added Sugars: The Main Inflammatory Culprits
The real troublemakers for inflammation are added sugars and refined sugars. These are the sugars that have been stripped from their natural source and pumped into countless foods and drinks to make them sweeter or last longer on the shelf.
You'll find these inflammatory sugars hiding in plain sight:
- High-Fructose Corn Syrup (HFCS) is a staple in sodas, processed snacks, and even condiments like ketchup.
- Sucrose (table sugar) is loaded into baked goods, candy, and sweetened teas and coffees.
- "Hidden" sugars lurk in foods you might not expect, like yogurt, pasta sauce, and salad dressings.
Because they've been isolated from any fiber or nutrients, these sugars hit your bloodstream almost instantly. This rapid-fire absorption triggers the sharp blood sugar and insulin spikes that we know are direct drivers of inflammation.
How Fructose Overwhelms Your Liver
There's a big problem with added sugars, especially high-fructose corn syrup, and it centers on your liver. While your body's cells can use glucose for energy, large doses of fructose have to be processed almost exclusively by the liver. When you chug a sugary soda, you're essentially flooding your liver with more fructose than it can handle.
Overwhelmed, the liver starts converting that excess fructose into fat. This process not only contributes to serious conditions like non-alcoholic fatty liver disease but also spins off inflammatory byproducts, adding even more fuel to the fire. For a deeper dive, check out our article explaining the difference between glucose and fructose.
One study showed that consuming just 25 grams of free sugar (the kind not bound up in whole foods) per day was linked to a 22% reduction in a type of immune cell that helps keep chronic inflammation in check. It's a powerful reminder of how even moderate amounts can weaken our defenses.
Why Natural Sugars Are Different
So, what makes the sugar in a handful of berries so much better? It’s all about its natural packaging. Whole foods provide a powerful combination of fiber, water, and nutrients that completely changes the game.
- Fiber is the superstar here. It dramatically slows down digestion, which means sugar enters your bloodstream gradually, preventing the inflammatory spikes you get from a soda.
- Water in fruit helps you feel full, making it much harder to overdo it on sugar compared to drinking empty calories.
- Antioxidants and phytonutrients found in fruit are nature's anti-inflammatory agents, actively working to calm inflammation in your body.
This brilliant combination ensures that sugar from whole foods provides a slow and steady stream of energy, all without triggering your body's inflammatory alarm bells.
The table below breaks down how different sugar sources stack up, clearly showing why reaching for a whole food is always the better choice for keeping inflammation at bay.
Comparing The Inflammatory Impact Of Different Sugar Sources
Here’s a comparative look at common sugar sources and their relative potential to cause inflammation in the body.
| Sugar Source | Primary Sugar Type | Inflammatory Potential (Low to High) | Key Reason |
|---|---|---|---|
| Soda | High-Fructose Corn Syrup | High | Rapid absorption, no fiber, overloads the liver. |
| Candy | Sucrose, Corn Syrup | High | Lacks nutrients and causes sharp insulin spikes. |
| White Bread | Refined Carbohydrates | Moderate to High | Quickly converts to glucose, stripped of fiber. |
| Whole Apple | Natural Fructose, Glucose | Low | Packaged with fiber, water, and nutrients. |
| Berries | Natural Fructose, Glucose | Very Low | High in fiber and anti-inflammatory antioxidants. |
As you can see, the context in which you consume sugar is everything. Choosing sources that are as close to their natural state as possible is a foundational strategy for managing inflammation.
The Health Risks of Long-Term Sugar Inflammation
Think of chronic inflammation from a high-sugar diet as a low, persistent hum of static in your body's communication system. It’s not an immediate, five-alarm fire. Instead, it’s a constant, low-grade stress that slowly wears down your internal machinery, year after year.
A single donut isn't the problem. But when your body is always trying to manage the inflammatory fallout from excess sugar, it’s like a repair crew that’s permanently on-site. Instead of just fixing immediate problems and leaving, they start getting in the way, causing system-wide disruptions that can lead to some serious health consequences down the road.
The Connection to Type 2 Diabetes
One of the first systems to feel the strain is your body’s ability to manage blood sugar. As we've discussed, high sugar intake triggers constant spikes in insulin. Chronic inflammation throws a wrench in this process, making your cells less responsive to insulin’s message. This is a dangerous condition called insulin resistance.
Imagine insulin is a key, trying to unlock your cells to let glucose in for energy. With insulin resistance, the locks get rusty and stiff. Your pancreas has to work overtime, producing more and more keys just to get the doors open. Eventually, the pancreas can get exhausted and burn out. When it can’t keep up, sugar stays trapped in your bloodstream, leading directly to type 2 diabetes. Sugar-fueled inflammation is a primary culprit in rusting those locks.
Damaging Your Heart and Blood Vessels
Chronic inflammation is also incredibly harsh on your heart and arteries. It acts like sandpaper on the smooth, delicate inner lining of your blood vessels. This constant friction creates tiny nicks and scratches.
These damaged spots become sticky patches where cholesterol and other substances start to build up, forming dangerous plaques. This process, called atherosclerosis, makes your arteries narrow and rigid. It’s a double-whammy for your heart:
- It has to pump much harder to push blood through the narrowed pipes, leading to high blood pressure.
- The plaques can break off, forming clots that can block blood flow to the heart (causing a heart attack) or the brain (causing a stroke).
A diet high in added sugar can increase the risk of dying from heart disease by over 38%, even if you aren't overweight. That statistic really drives home that sugar's inflammatory damage is a direct threat, independent of body weight.
The Strain on Your Liver
Your liver is the body's main processing plant, and it takes a direct hit from excess fructose, a common component of added sugars. When you flood your system with more sugar than you can use for energy, the liver has no choice but to convert that excess into fat.
This fat starts to build up in the liver cells, leading to non-alcoholic fatty liver disease (NAFLD). This condition makes the liver inflamed and stressed. Over time, NAFLD can lead to serious scarring (cirrhosis) and even liver failure. It's a key component of a cluster of issues, which you can read about in our guide to what is metabolic syndrome.
Beyond Major Organs
The damage doesn't stop with your heart and liver. Since inflammation is a body-wide problem, its effects can pop up in some surprising places:
- Joint Pain: It can pour fuel on the fire of arthritis, making joints feel stiffer and more painful.
- Skin Issues: Inflammatory skin conditions like acne and even premature aging are often linked to what's happening inside.
- Cognitive Decline: New research is drawing a strong line between chronic inflammation and a greater risk for neurodegenerative diseases later in life.
Seeing just how widespread these health risks are is often the motivation we need. The answer to "does sugar cause inflammation?" is a resounding yes, and understanding the long-term price is the first step toward reclaiming your health.
A Practical Plan to Reduce Sugar and Inflammation
Knowing the link between sugar and inflammation is one thing, but actually doing something about it is where the real health changes happen. The good news? You don't have to turn your life upside down overnight. Small, consistent changes can make a massive difference in your sugar intake, helping to calm inflammation and put you back in the driver's seat.
This plan is all about progress, not perfection. We'll start by showing you how to find the sneaky sugars that get in the way of your goals, then move on to simple swaps you can make today.

Become a Sugar Detective by Reading Labels
Your best tool for cutting down on sugar is right there on the package: the nutrition label. Food manufacturers are pros at hiding sugar where you'd least expect it, often using dozens of different names to throw you off. Learning to spot them is the key.
When you grab a packaged food, flip it over to the "Nutrition Facts" panel. The line for "Added Sugars" is your new best friend. This number tells you exactly how much sugar was put in during processing—the kind most directly linked to inflammation. A great rule of thumb is to look for products with 5 grams of added sugar or less per serving.
Next, give the ingredients list a quick scan. Since ingredients are listed by weight, seeing sugar near the top of the list means the product is packed with it. You'll also want to keep an eye out for sugar's many disguises.
- Syrups: High-fructose corn syrup, brown rice syrup, maple syrup, agave nectar
- Words ending in "-ose": Dextrose, fructose, sucrose, maltose, lactose
- So-called "natural" sugars: Cane juice, fruit juice concentrate, honey, molasses
Remember, even "natural" sweeteners like honey or agave nectar count as added sugars. While they might have trace nutrients, your body processes them pretty much the same way it does table sugar, which can fuel inflammation when you overdo it.
Make Smart Swaps to Reduce Sugar Effortlessly
You don't have to give up entire food groups. It’s all about making smarter choices. The goal here is to swap high-sugar items for lower-sugar alternatives that are just as tasty and satisfying.
Making these simple exchanges can cut a surprising amount of sugar from your diet without that feeling of deprivation. Think of it as an easy win in your fight against inflammation.
Easy Food and Drink Swaps
| Instead of This High-Sugar Choice... | Try This Lower-Sugar Alternative... | Why It Works |
|---|---|---|
| Sweetened Yogurt | Plain Greek Yogurt with fresh berries | You get natural sweetness from whole fruit, plus protein and fiber to keep you full and avoid blood sugar spikes. |
| Sugary Breakfast Cereal | Oatmeal with cinnamon and nuts | Oatmeal gives you slow-burning energy, and cinnamon can actually help regulate blood sugar. |
| Soda or Sweet Tea | Sparkling Water with a squeeze of lemon or lime | You still get that satisfying fizz but without any of the inflammatory added sugars. |
| Store-Bought Salad Dressing | Olive Oil and Vinegar | You skip the hidden sugars and unhealthy fats that are packed into most commercial dressings. |
Looking for other ways to cut back? It can be helpful to rethink your recreational drinks, too, since many cocktails and social beverages are loaded with sugar. For example, options like sugar-free THC drinks can offer a way to unwind without the inflammatory sugar load.
Actionable Tips for Sustainable Change
Building new habits takes time, so the key is to start with small, manageable steps you can actually stick with. Here are a few tips to get you going on your journey to reduce sugar and fight inflammation.
- Clean Out Your Pantry: Go through your kitchen and identify the biggest culprits—soda, candy, packaged cookies, and sugary cereals. If they aren't in the house, you can't eat them. Stock up on healthier alternatives like fruit, nuts, and seeds instead.
- Rethink Your Drink: Sugary beverages are one of the single largest sources of added sugar in our diets. Try to make water your go-to drink. If you need a little flavor, infuse it with fruit, mint, or cucumber. Unsweetened tea and black coffee are great choices, too.
- Focus on Whole Foods: Whenever possible, build your meals around whole, unprocessed foods like vegetables, fruits, lean proteins, and healthy fats. These foods are naturally low in sugar and packed with the anti-inflammatory nutrients your body needs.
- Cook More at Home: When you cook for yourself, you have complete control over what goes into your food. This is the easiest way to avoid the hidden sugars that are so common in restaurant meals and takeout. Just start with one or two simple recipes a week and build from there.
By becoming a label-reading pro, making smart swaps, and adopting these simple habits, you can seriously reduce your sugar intake. Consider this your roadmap to lowering inflammation and taking a huge step toward better long-term health.
Lifestyle Habits That Help Fight Inflammation
Cutting back on sugar is a massive step in the right direction, but your diet is only one piece of the anti-inflammatory puzzle. To truly answer the question "does sugar cause inflammation?" with real action, you need a lifestyle that supports your goals. Other daily habits work hand-in-hand with your food choices to create a powerful, cumulative effect.
Think of it like tending a garden. Kicking sugar to the curb is like pulling the weeds, but you still need to give the soil plenty of water and sunlight. Things like consistent exercise, quality sleep, and keeping stress in check are the other essentials that help your body thrive and keep inflammation from creeping back in.
Move Your Body to Reduce Inflammation
You have one of the most effective anti-inflammatory tools at your disposal: moderate, consistent exercise. You don't have to train for a marathon. Just getting out for a brisk, 30-minute walk most days can make a huge difference in lowering inflammatory markers.
When you get moving, your muscles release compounds that directly counteract chronic inflammation, especially the kind fueled by a high-sugar diet. It also gets your blood flowing, helps your body manage blood sugar, and supports a healthy weight—all of which create a less inflammatory environment inside you.
Prioritize Restorative Sleep
Sleep is prime time for your body’s repair crew. When you don't get enough quality rest, it puts your whole system under stress, throwing hormones out of whack and ramping up the production of inflammatory cytokines. It’s a big reason why you might feel achy and rundown after a bad night.
Chronic sleep deprivation can undo the hard work of even the healthiest diet. Aiming for 7-9 hours of solid, uninterrupted sleep each night is non-negotiable for keeping your body’s inflammatory response in check.
Small changes can have a big impact here. Sticking to a consistent sleep schedule (even on weekends), making your bedroom dark and cool, and ditching screens for at least an hour before bed can work wonders. You might also find that exploring the lemon verbena health benefits can add a naturally calming element to your wind-down routine.
Manage Your Daily Stress Levels
Being under constant stress keeps your body stuck in "fight-or-flight" mode, which means it’s constantly flooded with the stress hormone cortisol. In short bursts, cortisol actually fights inflammation. But over time, your body can become resistant to its effects, letting inflammation run wild and making the damage from sugar even worse.
Finding healthy ways to decompress is critical.
- Mindfulness and Meditation: Just 10 minutes a day can make a real difference in calming your nervous system.
- Spending Time in Nature: Getting outside is a proven way to lower cortisol levels.
- Gentle Movement: Activities like yoga or a simple stretching routine can release physical tension and ease your mind.
By bringing these habits into your life, you're building a complete strategy. You’re not just fighting inflammation from one angle; you’re tackling it from all sides and amplifying all the good you’re doing by eating less sugar.
Common Questions About Sugar and Inflammation
It's natural to have a ton of questions when you're untangling the connection between sugar and your health. Getting good, clear answers is the first step toward making choices you can feel confident about. Let's tackle some of the most common ones that come up.
How Quickly Will I Actually Feel a Difference?
While everyone's body is a little different, many people are surprised by how quickly they start feeling better. It's not uncommon to notice less joint stiffness, more consistent energy throughout the day, or even clearer skin within just a few weeks of cutting back on added sugars.
And that's just on the outside. Inside your body, the changes can happen even faster. Key blood markers for inflammation, like C-reactive protein (CRP), can start to drop in as little as two to four weeks when you stick with the changes.
Are Artificial Sweeteners a Good Swap?
This is a tricky one, and the answer isn't a simple yes or no. Since artificial sweeteners don't contain sugar, they won't cause that direct inflammatory spike from a blood sugar surge. But the story doesn't end there, and the long-term effects are still under a lot of scientific scrutiny.
Some studies suggest that certain artificial sweeteners can throw your gut microbiome out of whack. A healthy, balanced gut is one of your body's best defenses against inflammation, so this could be a significant downside. It's probably best to use them sparingly as you work on taming your sweet tooth overall.
Think of artificial sweeteners as a temporary bridge to get you away from sugar, not the final destination. The real goal is to start appreciating the natural sweetness in whole foods again.
What About the Sugar in Whole Fruits? Does That Cause Inflammation?
For almost everyone, the answer is a clear no. The sugar in a piece of whole fruit is completely different from the sugar in a cookie. It comes naturally packaged with fiber, water, and a host of powerful antioxidants.
This natural bundle is the secret sauce. The fiber dramatically slows down how quickly the sugar enters your bloodstream, which prevents the sharp, inflammatory spikes you get from processed, "free" sugars. The key is to always choose the whole fruit over fruit juice—juicing strips out that all-important fiber, leaving you with little more than a concentrated sugar rush.